2020 Pediatric Board Review Sneak Peek
Your 2020 Pediatric Board Review PREVIEW (and Discounted PREORDER Code) Is Here!

For non-members who are trying to figure out how they will approach the board exam, or for anyone preparing for the MOC (or for MOCA-Peds), this is a great opportunity to essentially have a sneak peak into the 2020 edition.
In this article, you will:
- Get a preview of the most EFFICIENT 2020 pediatric board review course available
- Get a great review of several excellent and high-yield topics
- Get a FREE MP3 Audio Chapter from PBR
- Get 50 FREE High-Yield Images from PBR
- Get a FREE Test-Taking Strategies Video Training Session
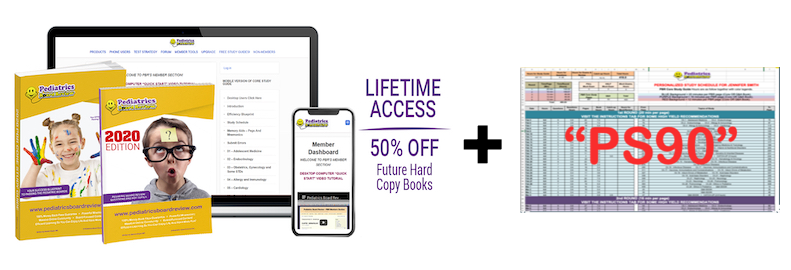
- Get the opportunity to PREORDER the 2020 edition books for 50% off of the value of the Ultimate Bundle Pack or 85% OFF of the LIFETIME package called “PBR FOR LIFE!” Please note that the PBR FOR LIFE package is NOT typically available through the PBR catalog, so this is a SPECIAL opportunity!
A FEW WORDS OF THANKS TO THE PBR COMMUNITY
Every year I like to go through all PBR error submission and send corrections to PBR members before the initial certification exam. It’s an EXTREMELY time consuming task (takes weeks), but it’s worth it.
Although the information in this guide SHOULD NOT make or break your test-experience if you have followed, THE PBR EFFICIENCY BLUEPRINT, several test-takers have previously said that these corrections and clarifications have helped them correctly answer questions that came up on the exam.
THANKS TO YOU!
- Thank you to EVERYONE who submitted spelling errors, typographical errors, corrections or requests clarifications from within the PBR by visiting the ERROR page:
www.pediatricsboardreview.com/error
For everyone who provided a page number, a clear question and a reference – oh my goodness… you rock!
- Thank you to EVERYONE who submitted broken links from within the PBR and the PBR Picture Atlas by visiting the BAD LINK page:
www.pediatricsboardreview.com/badlink
- An absolutely MASSIVE THANKS TO DR. JOHN COLE! John is a PBR alum, he’s been an OVC Summertime Q&A Webinar panelist and he’s also taken on the role of being PBR’s editor! He has a HUGE heart, and he acts as our editor to help you and the PBR community.
- A huge thanks to our 2019 Online Video Course Summertime Webinar speakers. They contributed to MANY of the chapter corrections or revisions!
- Amar Dave
- John Cole
- Asalim Thabet
- Kara Wada
- Shamila Zawahir
- Arpit Agarwal
- Lina Huerta-Saenz
- Stephanie Moses
- Kirshma Khemani
- Moshe Cohn
- Raza Bajwa
NOW… WHAT IS THIS THING?
We like to address as many concerns about the PBR content BEFORE the initial certification boards in October.
IN ORDER OF PRIORITY, OUR FOCUS HAS BEEN….
- Addressing error submissions from the PBR Error portal (www.pediatricsboardreview.com/error). Basically, stuff where folks are saying,“Ashish… I think (or I know) that this is wrong. You should fix it in the book and let folks know about it because it’s more than just a spelling or grammar issue.”
- Addressing questions from our Online Video Course question portals and webinars. The summer is filled with content-based webinars, and many excellent questions, corrections and clarifications come to light during those sessions. We try to address as many of those as possible before the Initial Certification Exam.
- Addressing possible errors/concerns mentioned in the PBR Facebook CREW! Yes… We kind of “stalk” the group and if I see something comes up that might warrant a correction in the PBR. I set it aside for this time of year to review.
- Requests for content clarification through the portal or “The CREW”.
In general, the “PBR Facebook CREW!” is meant to help you get the help you need to understand a topic. BUT, if I see that there’s a topic that could be explained better based on CREW conversation, I make a note of it and try to polish it up for the next edition and address the issue in this guide.
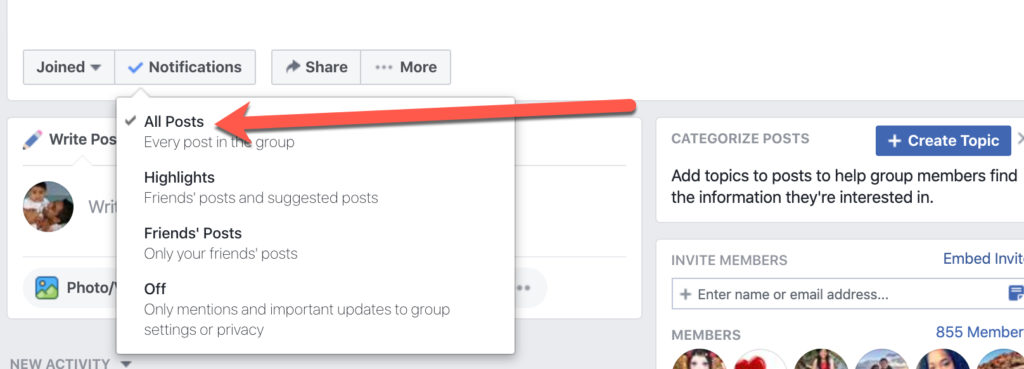
Because the PBR membership continues to grow, there has been EXCELLENT chatter in “The PBR Facebook CREW.” If you are a member of the “The PBR CREW” but you have NOT been seeing all of the posts, please visit the private group and make sure that your NOTIFICATION SETTINGS ARE SET TO ALL POSTS. This is critical!
ARE YOU NERVOUS BECAUSE THERE ARE CORRECTIONS FOR THE PBR CONTENT?
ALL study guides have errors! I’m simply the only author who is crazy enough, and passionate enough, to take on something like this prior the boards every year so that you can rest EASY. And instead of just giving you a one page errata sheet based on error submissions, we try to go much deeper in our explanations and we also SEEK OUT areas of improvement to share with you.
For some people, though, the idea that the PBR has errors can be anxiety provoking.
If you’re one of those members, please keep in mind that there are OVER 2000 topics within the PBR, and each topic has MANY salient points associated with it. There are probably over 10,000 individual pieces of information in the PBR. Therefore, the number of corrections below is relatively TINY.
So you should rest easy knowing that there is MORE THAN ENOUGH excellent content within your PBR to get you your PASS! The PBR CERTIFICATION SYSTEM has helped pediatricians get ABOVE the national average score after MULTIPLE years of failing with other resources… so you’ll be fine!
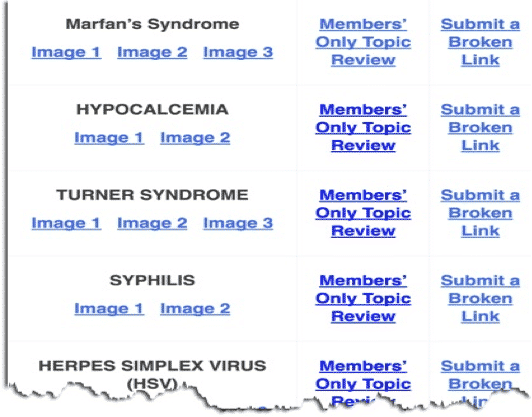
WHAT ABOUT IMAGE LINK CORRECTIONS?
We have a very innovative system that allows you to view phenomenal high-yield images across the web. We have approximately 400 image links in the PBR, but they lead to images that are not owned by PBR. That means that any given time, an unrelated PBR website that houses a high-yield image might be down. When you notify us of this, it’s a HUGE help and we can quickly replace the image link with a new, comparable image.
In the past we would send out replacement image links for the ones that were broken throughout the web. Because of our new systems, all of the image link corrections now happen on the BACKEND.
We just did a huge search and replace of the links. 97% – 99% of the links should now be working without any issues!
If you do find that there’s an issue, please notify us immediately by visiting: www.pediatricsboardreview.com/badlink
The EASIEST way to go through all of these images is by using the online picture atlas created by Team PBR (called the Virtual Atlas of Pediatric Pictures). The VAPP gives you a SUPER fast and high-yield review of board-relevant images.
You can watch the video below to see how it works:
www.PediatricsBoardReview.com/vapp
GET ACCESS TO 50 FREE IMAGES BY CLICKING THE PICTURE BELOW!
FREQUENTLY ASKED QUESTIONS
“Is this a complete list of everything that’s changing for the new edition?”
NO. The new edition will have MORE additions and modifications. This Corrections & Clarifications Guide includes:
- Clarifications and discussions around topics that may have been confusing to readers, or to attendees of our Live Summertime OVC Q&A Webinars
- A set of absolute notifications because they were true errors that we verified.
There are more submissions that we need to do additional research on, and NEW submissions for consideration that are still coming in. Those will likely result in additional changes to the next edition.
“I’m taking the exam NEXT YEAR. If I have the old book… Should I keep that one or get the new one?”
Your older edition likely has enough information in it to help you pass the initial certification (or recertification) exam. BUT, we are adding new information (new topics, new subtopics, and possibly even a new section, etc.) based on member feedback.
Here are the 6 main reasons to get the new edition if you still have an old one:
- IT’S FRUSTRATING TO HAVE AN OLDER BOOK. WATCH!
- You will see in this guide that many submissions will reference specific page numbers and specific lines within a paragraph. This happens all year long, especially in our private forum. This is NOT the time to be spending your energy cross-checking everything in this guide against your older version of the PBR. Your time is PRECIOUS and needs to be spent EFFICIENTLY and effectively.
- Start with a fresh book, transfer any notes/drawings from your previous hardcopy to the new edition as you read through it the first time, and then use the new one as your bible! The purging of “the old” and the starting with “the new” is also a great MENTAL RESET.
- NEW CONTENT: There is ALWAYS new content in a new release. MANY of the corrections below were included in this guide because of help from the PBR community, and many were done on my own. But there are more corrections that need further investigated before the next edition’s release.
- NEW CLARIFICATIONS: There was ACTIVE discussion within the members’ only PBR Facebook CREW! about board review topics that I THOUGHT were explained well within the PBR. That discussion leads me to believe that I can be EVEN MORE clear in future editions. There will be many additional clarifications and updates in the next edition.
- COST (No… I’m not just talking about money!)
- By cost, I mean money and opportunity cost. The cost of a new book is minimal compared to the hard financial cost and the opportunity cost of FAILING the boards. The financial cost of FAILING includes over $2000 for your board fees, plus the cost of taking time off of work to study again next year (THOUSANDS of dollars of lost income). You also must include the stress and the time away from loved ones as a tremendous unmeasurable cost.
- If you’re planning on using the older version due to financial concerns, that’s actually pretty silly. As your guide on this journey, I feel that it’s important that I be blunt when it comes this point. I have such a passion for efficiency and QUALITY USE OF TIME that it really pains me to hear about physicians that are trying to go back and forth between the corrections guide and their old study guide in order to save a few dollars. Plus, having a NEW and CLEAN book that you can start going through with my highlighter trick is a much better means of achieving DEEP STUDY.
- REFERENCES TO PBR IN THE CREW!
- The PBR Facebook CREW comes alive with discussion as the boards approach. Many PBR alumni have said that the Facebook CREW! heavily contributed to their success on the boards. When your peers in “The CREW” are referring to a topic on a certain page, do you really want to (again) waste your precious time fumbling around and trying to find the topic they’re referring to?
- UPGRADED FORMATS: Every edition is MUCH better than the previous.
- Corrections
- Clarifications
- New image links
- NEW, TIMESAVING INNOVATIONS. For example, our links used to be EXTREMELY long. Now we have a system that turns http://upload.wikimedia.org/wikipedia/commons/4/45/Aphthous_ulcer.jpg into something easy like pbrlinks.com/aphthous1. HOW COOL IS THAT! Try typing out the 2 different links and see HOW FAST you get to review images using the new PBR link – these things get me SO EXCITED!
DISCLAIMERS/WARNINGS
PLEASE READ THIS BEFORE YOU GET STARTED
- The page numbers in this guide refer to the 2019 Editions of the Pediatrics Board Review books (covers shown below).
- DEAR NON-PBR MEMBERS… the PBR Facebook CREW! is a private, members-only area for anyone who has signed up for a qualifying product. YOUR REQUEST TO JOIN WILL BE REJECTED if you have only signed up to get free info from PBR (free GI & DERM study guides, free emails about new PBR web article, free Q&A discounts, free MP3, etc). We cross-check all requests to join “The CREW” before clicking the APPROVE button. This is done in order to keep it a spam-free, private and intimate area.
- Reminder… I LOVE being told I’m wrong (sort of), so keep the comments coming! Just keep in mind that the best place to submit error submissions, corrections, requests for clarifications, etc. is here:
LET’S GET STARTED WITH THE CORRECTIONS FIRST!
OKAY…. This first section is going to cover TRUE ERRORS that were in the PBR and possibly some clarifications that are going to result in CHANGES for the next edition.
Got more errors to submit? Send them over!www.pediatricsboardreview.com/ERROR
ADOLESCENT MEDICINE
p. 57, menarche bullet point. “Amenorrhea does not require workup until 2 years after puberty has ended. How could have it ended if menarche didn't happen? Does that make sense?
- This is a little confusing. The idea is that amenorrhea does not require workup until 2 years after puberty has ended. Since puberty may take 5 years to complete, it’s possible a patient may not need a workup for amenorrhea until 7 years after their breast buds form.
- We will delete this sentence and replace with the following scenarios:
- A workup for amenorrhea/delayed puberty should be completed if no menses occur after the breast contour changes from a mound on mound type of breast appearance to a round appearance (SMR 5), or a lack of menses within 2 years of any true breast development, or no signs of puberty or menses by age 14 (if starting to have breast development at 13 or 14 years old, can wait 2 years prior to workup).
==========================================
ENDOCRINOLOGY
p.85 – under the section HYPOGLYCEMIA, neonatal bolus rate for D10 is marked as 2.5 ml/kg at rate of 2-3 mil/min; p.167 – under the section NEONATAL HYPOGLYCEMIA, neonatal bolus rate for D10 is marked as 2 ml/kg, but your calculation in the same section was (a) missing units (needs to be 8 ml/kg, not just 8 ml); but also (b) was based on a rate of 2.5 ml/kg (avg baby wt 3.25kg, rate 2.5 ml/kg). So I think what you meant to write here was a rate of 2.5 ml/kg? Please adjust this discrepancy on p.167 if that is correct.
- Yes, there is a discrepancy here. But for (a) the ml/kg doesn’t belong. I’ve updated it below for more clarify. For (b), also see below. 3.25 kg * 2 ml/kg = 6.5 ml of D10.
- “For infants and young children give 2 ml/kg of D10 (max dose is 500 ml, which equals 50 g of dextrose).” -p.85
- “For an average sized newborn, that is 6.5 ml of D10 (3.25 kg x 2 ml/g).” -p.167
- “If the hypoglycemia is persistent, or recurrent, consider an IV infusion rate of D10 at 80 ml/kg/hr.” – p.167
==========================================
OB/GYN and some STD’s
On page 90 of the current version, it states that Chlamydia is the most common STD; however, HPV is the most common STD, while chlamydia is the most common reportable STD.
- Yes, HPV is the most common STD. Most frequently REPORTED STD is Chlamydia. Most common BACTERIAL STD is Chlamydia. See updated text below.
- (Double Take) Chlamydia trachomatis
Chlamydia trachomatis can cause urethritis, conjunctivitis and pelvic inflammatory disease (PID). In neonates, it can cause pneumonia associated with a staccato cough. PID can lead to ectopic pregnancies and infertility. Eye infections can lead to blindness. Conjunctivitis in a neonate (less than a month old) should raise concern for this as the etiology (vertical transmission). It’s an obligate intracellular anaerobe. Getting cultures is difficult, so order PCR of CELLS, secretions, or urine. Chlamydia can also cause lymphogranuloma venereum (LGV), which is an STD that initially starts with small, nontender papules or shallow ulcers that resolve. Then a TENDER UNILATERAL INGUINAL lymph node appears that can rupture, relieve the pain, and then possibly drain for months.
SEXUALLY TRANSMITTED DISEASE (STD): Treat with Azithromycin x 1. If cost is a concern, then treat with DOXYCYCLINE for 7 days. If the patient is given doxycycline and there is recurrence, treatment failure, or a concern for noncompliance, treat with AZITHROMYCIN x1. Other possible medications include erythromycin, levofloxacin, or ofloxacin for multiple doses/day x 7 days. Test for other STDs including gonorrhea, syphilis, and HIV and treat if positive.
CONJUNCTIVITIS: Treat with oral erythromycin to eradicate nasopharyngeal colonization, which can lead to pneumonia.
* (DOUBLE TAKE) LYMPHOGRANULOMA VENEREUM SEROVAR
Lymphogranuloma Venereum Serovar is an STD caused by Chlamydia trachomatis. It is rare in the U.S. but more common in tropical areas. It starts as small nontender papules or shallow ulcers that resolve. Eventually, a TENDER UNILATERAL INGUINAL lymph node appears. Pain is relieved when it ruptures. The node can continue to drain for months. Treat with DOXYCYCLINE or erythromycin.
* PEARL: In general, when you think the diagnosis is due to a Chlamydia species, choose doxycycline if the child is > 8 years of age, or choose a macrolide (usually erythromycin). Also, this is an intracellular organism.
* PEARL: Lastly, while chlamydia is often said to be the most common STD, that’s not the case. It’s the most common BACTERIAL STD, and it’s the most commonly REPORTED STD. HPV is the most common STD.
==========================================
ALLERGY AND IMMUNOLOGY
Is it true that the only vaccine that is contraindicated in those with anaphylaxis to egg is Yellow Fever?
- Yes. The yellow fever vaccine tends to be contraindicated in many immunodeficiencies and those with anaphylaxis to egg.
- The live attenuated influenza vaccine (LAIV, FluMist ®) can be given with severe allergic reactions to eggs, chicken, or gelatin. This will be removed from the text on page 322. (https://www.cdc.gov/flu/prevent/egg-allergies.htm and https://www.uspharmacist.com/article/pharmacists-dont-need-to-ask-about-egg-allergies-before-flu-shot)
==========================================
CARDIOLOGY
Under rheumatic fever associations, it says right-sided diastolic murmur of aortic regurgitation—this in incorrect. Aortic regurg murmur is apical diastolic murmur whereas the aortic stenosis murmur is RUSB diastolic
- Yes, you are correct. We mention, “right-sided diastolic murmur of aortic regurgitation” on page 130. This should instead say apical diastolic murmur of aortic regurgitation. Thank you!
Under rheumatic fever associations on page 130, the 2nd to last bullet point reads “Endocarditis occurs due to destruction of valves, NOT infection.” Then on page 131 under endocarditis definition the 1st sentence reads “Endocarditis is defined as an infected heart valve.” Please clarify if this is the case because otherwise the two definitions seem to contradict one another.
- Excellent, good catch! The CSG will be updated as seen below.
- Endocarditis is defined as inflammation of the endocardium or heart valves. This is usually caused by an infection (infective endocarditis) but can occur with other conditions in which there is no active infection. Examples of noninfective endocarditis include Libman–Sacks endocarditis due to systemic lupus erythematosus and endocarditis due to rheumatic fever. In general, STREP VIRIDANS is the most common etiology of infectious endocarditis in children, followed by Staph aureus and then Staph epidermidis (especially if the valve is prosthetic).
Regarding the treatment of WPW on page 133, the last paragraph under WPW starts with tx as SVT but that Beta Blockers should be avoided but SVT is treated with propranolol for a year. Is it no Beta Blockers if there is no SVT with WPW?
- Treatment for WPW varies depending on if we’re talking about the acute treatment at the time of presentation versus chronic treatment. If a patient presents with SVT, then adenosine is given during this acute event. Once the acute event has resolved, the longterm treatments may include beta-blockers, calcium channel blockers, and possibly EP ablation.
- We will add a line to the CSG that says: For the chronic treatment of WPW, options include beta-blockers, calcium channel blockers, and possibly EP ablation.
Regarding myocarditis on the bottom of page 133 – I heard that tachycardia is a frequent symptom, but it’s not mentioned in the Core Study Guide (CSG).
- Yes, you are correct. The CSG will be updated as seen below.
- For myocarditis, tachycardia (sinus tachycardia or an arrhythmia) is often the presenting symptom. Also look for fever, chest pain, sudden heart failure symptoms (gallop, hepatomegaly, splenomegaly), pulsus paradoxus, or a combination of these.
Is Staph Aureus or Strep Viridans the #1 cause of endocarditis?
- Depends…among children WITH underlying heart disease Strep viridans accounts for 33% of causes of IE vs. Staph aureus which accounts for only 28% of disease. However, among children WITHOUT underlying heart disease, Staph aureus accounts for 47% of cases vs. Strep viridans which only accounts for 18% of cases of IE.
- https://www.uptodate.com/contents/infective-endocarditis-in-children
- This will be clarified in the new version of the CSG.
Pg.76, pg..349 – Late hypocalcemia – one of the etiologies that is correctly listed is hypomagnesemia. However, on pg. 116 under “PROLONGED QT,” part of the sentence reads as “…caused by hypomagnesemia (which can be caused by hypocalcemia)…” –> I think this was written backwards; I think you meant to say “…caused by hypomagnesemia (which can lead to hypocalcemia)” –correct?
- Yes, you are correct, there is an error. Chronic hypomagnesemia can result in hypocalcemia due to decrease in PTH.
==========================================
DERMATOLOGY
No Corrections! But the 2020 Pediatrics Board Review Study Guides May Have New Content (Or Corrections).
==========================================
NEONATOLOGY
Error about rhogam on page 165 – Rhogam is given at 28 weeks (not 20 weeks) and after delivery
- You are correct. It should be 28 weeks.
- (DOUBLE TAKE) RHESUS DISEASE (AKA RH DISEASE). When checking for Rhesus Disease (AKA RH Disease), look for an Rh- mom in her SECOND pregnancy: Maternal IgM antibodies are made during the FIRST pregnancy and are too large to cross over into the fetal circulation. During the SECOND pregnancy, IgG antibodies are present that are small enough to cross. (This can cause ERYTHROBLASTOSIS FETALIS if they cross early in pregnancy.) Rh- moms are supposed to get RHOGAM at 28 weeks’ gestation, and then again after delivery if the baby is found to be Rh+.
- https://www.acog.org/Patients/FAQs/The-Rh-Factor-How-It-Can-Affect-Your-Pregnancy?IsMobileSet=false
The book, 9th ED, P 164 says that screening for ROP is for “.. all kids <1500g OR < 32 weeks should be screened for ROP.” This is incorrect. It should be < 30 weeks.
- Yes, < 30 weeks or < 1500 g is correct. https://pediatrics.aappublications.org/content/pediatrics/early/2018/11/21/peds.2018-3061.full.pdf
- RETINOPATHY OF PREMATURITY (ROP): According to the AAP, all kids < 1500 g OR < 30 weeks should be screened for Retinopathy of Prematurity (ROP). The greatest risk is for kids born at < 29 weeks gestation or who have a birth weight of < 1200 g. The first retinal exam is scheduled based on the gestational age at birth. For a gestation age of 27–30 weeks at birth, the first exam is at 4 weeks of chronologic age. I suspect this is a low-yield fact.
==========================================
DEVELOPMENTAL MILESTONES
No Corrections! But the 2020 Pediatrics Board Review Study Guides May Have New Content (Or Corrections).
==========================================
EMERGENCY MEDICINE AND TOXICOLOGY
CPR Guidelines – PBR Core Book 9th Ed.- p.201. Under Cardiopulmonary Resuscitation (CPR), the book says that double rescuer for babies and children has ratio of 15:1 compressions:breaths. I think it’s actually 15:2. Can you confirm?
Adolescents and up –> always 30:2
- You’re correct! The latest guidelines state that 1 cycle is 30 chest compressions to 2 rescue breaths for a single rescuer, and if there are two rescuers then 1 cycle is 15 chest compressions to 2 rescue breaths.
During my toxicology rotation at NY Poison Control, they taught us that unless acetaminophen ingestion goes above 200mg/kg, we can wait the 8 hours we have post-ingestion to give the NAC. I wanted to know if the 140mg/kg is specifically something we need to know for the boards but not real life? I brought up the 140mg/kg we learned in our review book but they said that's not necessarily something they typically recommend… so I'm wondering. Thank you.
- Yes, you are correct. See updated section below
- ACETAMINOPHEN INGESTION
In cases of acetaminophen ingestion, obtain an acetaminophen level at 4 hours post-ingestion and plot on the nomogram. Treat with N-acetylcysteine (NAC). NAC can be given by IV or PO. It acts as a glutathione precursor. If the number of tablets is known and the dose exceeds 150 mg/kg (children > 6 years old) or 200mg/kg (children aged 1-6 years old), treat with NAC immediately. Otherwise, you may WAIT until the level returns to plot it on the nomogram before giving the NAC, but it must be given within 8 hours of ingestion. So, if the level will not come back until after 8 hours post-ingestion, give NAC now.
==========================================
VITAMINS AND NUTRITIONAL DISORDERS
No Corrections! But the 2020 Pediatrics Board Review Study Guides May Have New Content (Or Corrections).
==========================================
GASTROENTEROLOGY
For Achalasia, gold standard of diagnosis in medstudy qbank states “esophageal manometry”… in our book it says upper GI series. Which is it? ….They're not the same right?
- To diagnose, first start with an upper GI barium series to look for a “bird’s beak” appearance. Then do an EGD to look for masses, or other abnormalities, that could cause the same appearance. Finally, the esophageal manometry (the gold standard test) is done to look for an absence of contraction and a high tone within the esophageal sphincter while the patient is asked to swallow.
==========================================
PHARMACOLOGY AND DRUG PEARLS
No Corrections! But the 2020 Pediatrics Board Review Study Guides May Have New Content (Or Corrections).
==========================================
OPHTHALMOLOGY
No Corrections! But the 2020 Pediatrics Board Review Study Guides May Have New Content (Or Corrections).
==========================================
GENETICS
No Corrections! But the 2020 Pediatrics Board Review Study Guides May Have New Content (Or Corrections).
==========================================
HEMATOLOGY AND ONCOLOGY
In the 9th edition, page 264-265, regarding: the treatment for spleen sequestration crisis in sickle cell anemia. PBR says Tx of choice is IVFs, HOWEVER the 𝐓𝐱 𝐨𝐟 𝐜𝐡𝐨𝐢𝐜𝐞 𝐢𝐬 𝐓𝐫𝐚𝐧𝐬𝐟𝐮𝐬𝐢𝐨𝐧 𝐰𝐢𝐭𝐡 𝐏𝐑𝐁𝐂𝐬. I just got a question with this in PREP 2017, and confirmed with the PIR article from 2012.
- Start off with IVF in the ED, but the official treatment would be transfusion of PRBCs. Ideally 5 ml/kg of volume. To decrease hyperviscosity syndrome after blood transfusion due to blood trapped in the spleen, a lower volume of PRBCs is used (typically 50%).
On page 275 under the “coagulation cascade” subheading it reads Factors III and VII are the main extrinsic factors. I think it is meant to be factor II instead of III.
- Actually, TF and VII are the main extrinsic factors. Good catch and thank you for the update.
- COAGULATION CASCADE
Factors XII, XI, and IX are the main INTRINSIC factors in the coagulation cascade and partially measured by aPTT. Tissue factor (TF) and factor VII are the main EXTRINSIC factors in the coagulation cascade and partially measured by the PT. Factor X is part of the common pathway.
=========================================
INFECTIOUS DISEASES
Toxocara is a roundworm, not a tapeworm. Your entry in your section on Hemoptysis (follows) states that Toxocara is a tapeworm, but instead it is a roundworm.
“MIGRATING PNEUMONIAS VISCERAL LARVA MIGRANS (DOUBLE TAKE) Toxocara canis is a tapeworm that causes VISCERAL LARVA MIGRANS. Look for a child presenting with multisystem complaints. Usually affects the LUNGS and the GI TRACT but can also affect the eyes. May present as abdominal pain in a child who has hepatosplenomegaly and wheezing on exam. Labs will show a HIGH LEUKOCYTOSIS with EOSINOPHILIA. Imaging will show lung infiltrates. The tapeworm is found in cats, dogs, and dirt …”
- You’re correct! Thanks. We’ll update page 299.
Pg. 305 Core Content Book and pg. 44 question pg. #39 answer. Regarding newborn Testing. Question answer notes “obtain FTA in the baby” but the book notes ” FTA on a baby is difficult to interpret so not recommended. Which is correct? Should a baby have FTA or RPR /VDRL done?
- The Core Study Guide is correct. FTA has fallen out of favor in recent years so an RPR/VDRL on the infant should be done.
In reference to PBR: “Early onset”: First 3 days of life. It is usually due to GBS pneumonia. “Late onset”: After 3 days and up until the first 90 days of life. Infections tend to be more focal. GBS Sepsis in PBR differentiates early vs late cut off as 3 days, in uptodate and medstudy qbank it says 7 days… please clarify if late onset sepsis >= 7 days or >=3 days.
- You’re correct! It looks like early onset can happen as late as 6 days. “Late onset” GBS sepsis refers to sepsis occurring after 6 days and up to the first 90 days of life.
For fluoroquinolones, the PBR says that they shouldn’t be given if < 18 yo. I've seen in questions – kid steps on rusty nail, punctures through rubber sole of shoe – if kid shows sign of infection, give ciprofloxacin to cover for pseudomonas.
- Good point! We’ll update the Core Study Guide.
- ERYTHROMYCIN: For erythromycin, do not use in children younger than 1 month of age due to an association with pyloric stenosis. Instead, use azithromycin.
For page 289 – for TB skin test: cutoff should be 5 to <10, 10 to <15, 15 or greater. That's what it says it RedBook. (PBR should show a >/=10, >/=15)
- You are absolutely correct! We believe that the boards would not give you the actual number where a specific range cuts off (5, 10, or 15), but this is an error that we’ll definitely fix for the next edition. Thanks for the submission.
For pages 295-296, Borellia & Leptospira are spirochetes – should be under gram neg bacteria section, not protozoa, right?
- Yes, you are correct, and this will be updated in the next version of the book.
==========================================
VACCINES, IMMUNIZATIONS AND CONTRAINDICATIONS
No Corrections! But the 2020 Pediatrics Board Review Study Guides May Have New Content (Or Corrections).
==========================================
INBORN ERRORS OF METABOLISM
p.330 – under FATTY ACID OXIDATION DISORDERS – the PEARL states: “If given an answer choice with a disease that has “CARNITINE” in the name of it, that IS a fatty acid oxidation disorder.” I think the word you were looking for was not “Carnitine,” but “Acyl-Co-A,” or “Acyl-coA dehydrogenase,” correct? Because all of these disorders (medium chain/long chain/very long chain acyl-coA dehydrogenase), have this word in it.” Please correct.
- Yes, you are correct. New text will read: “If given an answer choice with a disease that has “Acyl-Co-A dehydrogenase” in the name of it, that IS a fatty acid oxidation disorder.”
p.328 – under UREA CYCLE SUMMARY – this section is HARD to understand – I'll be frank. After much review and rechecking, it appears that the first bullet about the 1st step of the urea cycle is incorrect. It currently reads as “Ammonia and Ornithine (a urea cycle end product) present to Carbamoyl Phosphate Synthetase, which converts them into Citrulline using the catalyst Ornithine Transcarbamylase.”
–> it appears that this sentence combined the first 2 steps of the urea cycle (with 2 separate enzymes and metabolites) into 1 step.
–> The first 2 steps of the urea cycle are listed below (not including ATP or energy sources):
- Carbamoyl Phosphate Synthetase (CPS) converts Ammonium (NH4+) and Carbon Dioxide (CO2) to Carbamoyl Phosphate.
- Ornithine Transcarbamylase (OTC) converts Carbamoyl Phosphate and Ornithine (a urea cycle end product) to Citrulline.
Separating the steps as above makes MUCH more sense and is more accurate. And it's far easier to follow the steps since the names of the enzymes and metabolites help guide us and improve our recall of the steps.
Similarly, the last bullet of the section reads: “Ornithine Transcarbamylase then works again with Carbamoyl Phosphate Synthetase to catalyze the reaction between Ammonia and Ornithine to create Citrulline.”
–> again, this sentence is not correct because the 2 enzymes have 2 separate steps with separate metabolites as mentioned earlier; and the initial metabolite used is actually the Ammonium cation (NH4); Ammonia (NH3) is the end product as you mentioned, not in the beginning.
…(again I'm terribly sorry for being so nit picky, but adjustments/corrections like this would make it so much easier for us to understand the material and improve our recall).
- Good catch, appreciate the nit-picky-ness! We will update the new edition of the book with corrections on the first and last bullet in this section and add in the link that you suggested.
- Ammonium (NH4+) and Carbon Dioxide (CO2) combine with Carbamoyl Phosphate Synthetase (CPS) to form Carbamoyl Phosphate. Then, Ornithine Transcarbamylase (OTC) converts Carbamoyl Phosphate and Ornithine (a urea cycle end product) to Citrulline.
- Ornithine Transcarbamylase (OTC) then works again with Carbamoyl Phosphate and Ornithine to create Citrulline
- https://microbenotes.com/urea-cycle-enzymes-and-steps/
==========================================
ACID-BASE DISORDERS
No Corrections! But the 2020 Pediatrics Board Review Study Guides May Have New Content (Or Corrections).
==========================================
FLUIDS AND ELECTROLYTES
No Corrections! But the 2020 Pediatrics Board Review Study Guides May Have New Content (Or Corrections).
==========================================
NEPHROLOGY
According to Pedialink: The combination of a low C3 level and a normal C4 level indicates activation of the alternative pathway of complement and occurs in postinfectious GN or MPGN. However, on page 360 of PBR, it states that MPGN has low C3 and LOW C4…. is this a mistake? Thank you!
- The pedialink information is correct. There is an error in the PBR and the correct wording should be a low C3 and normal C4 for MPGN
- (DOUBLE TAKE) POST STREPTOCOCCAL GLOMERULONEPHRITIS (PSGN, AKA POST INFECTIOUS GLOMERULONEPHRITIS)
Post streptococcal glomerulonephritis (PSGN, AKA post infectious glomerulonephritis) is a Group A Streptococcus (GAS) syndrome. Look for HEMATURIA + PROTEINURIA ± swelling ± HTN. There may be a history of a skin infection one month before, or a throat infection 1–2 weeks earlier. Labs will show a low C3 and NORMAL C4 ± renal impairment. Biopsy will show LUMPY BUMPY IgG deposits (biopsy is not required to make the diagnosis). Treat with IVF and a loop diuretic if there’s HTN. This generally has a GOOD prognosis, but you may consider steroids or cyclophosphamide for cases that are not improving. C3 should be followed until it’s back up to normal.
PEARL: Antibiotics given for a Group A Strep infection can prevent rheumatic fever, but they CANNOT prevent PSGN. Also, PSGN can occur from pharyngitis OR skin infections, but rheumatic fever only occurs after PHARYNGITIS.
PEARL: If the C3 level does not come back up to normal after 6 weeks, consider a different diagnosis, such as membranoproliferative glomerulonephritis (MPGN has a low C3 and normal C4) or lupus nephritis (+ANA, low C3 and C4). If the renal impairment is severe, obtain a biopsy to look for rapidly progressive glomerulonephritis (RPGN).
- MEMBRANOPROLIFERATIVE GLOMERULONEPHRITIS (MPGN)
Membranoproliferative glomerulonephritis (MPGN) findings include hematuria, proteinuria, and high blood pressure. The key lab findings include a low C3 AND a normal C4. Confirmatory diagnosis is via biopsy showing TRAM TRACK lesions.
MNEMONIC: MEMBERS OF PARLIAMENT (MPGN) riding a TRAM on TRACKS leading to a circus LOOP OF FIRE. (LOOP = Lupus since SLE patients can get MPGN. Low-yield.)
ADTKD vs ADPKD – I just want to know that these two are different diseases, and not spectrum of the same disease. thank you
- These are 2 different entities. As stated in the Core Study Guide, ADTKD is low yield. ADPKD is a much more tested topic and we mention it a few times in the Core Study Guide but are now going to include the following topic in the new Core Study Guide as well:
- AUTOSOMAL DOMINANT POLYCYSTIC KIDNEY DISEASE (ADPKD)
Progressive multisystemic disorder involving cysts and enlargement of the kidney and other organs (liver, spleen, pancreas). Patients commonly present with pain in the flank, back, or abdomen and hypertension. Diagnose with ultrasound showing at least 2 cysts in 1 kidney or 1 cyst in each kidney in a patient under 30 years old. Genetic testing is not routinely performed, unless the patient is a potential kidney donor.
==========================================
STATISTICS
Can you please speak more about Hazard Ratios and Kaplan Meier curves – pearls? easy to remember concepts? I have seen questions on both in various Q-Banks. Only saw brief mention of Hazard Ratios in PBR and did not see anything on Kaplan Meier. Or are they low yield?
- The Kaplan-Meier Estimator (used to create Kaplan-Meier curves) is used to estimate survival. The X-axis will always have a time component, and the Y-axis will typically have “Percent Survival.” The estimate can be useful to examine the probability of death, the effectiveness of a particular treatment, and recovery rates.
- IMAGE: pbrlinks.com/kpcurve
- The hazard ratio is a low yield calculation. Just use what is in PBR. The hazard ratio is the ratio of hazard rates to the condition being studied. Hazard ratios represent the instantaneous risk over the study time period.
==========================================
NEUROLOGY
No Corrections! But the 2020 Pediatrics Board Review Study Guides May Have New Content (Or Corrections).
==========================================
ORTHOPEDICS AND SPORT MEDICINE
Guidelines have changed for developmental dysplasia of the hips. Please update. Question had a 1 day old girl, nml hip exam, mom with h/o DDH. options were referral to ortho, image at 2 months with XR, image with US at 6 weeks. I picked referral based on your pearl and they wanted US. I'm annoyed! did I miss understand the PBR reference guide? Ive missed two questions now 2/2 PBR
- You are correct and this entire section has been completely overhauled.
- DEVELOPMENTAL DYSPLASIA OF THE HIP (DDH)
Infants with developmental dysplasia of the hip (DDH) may be noted to have a leg-length discrepancy, extra creases at the thigh, “clunks” or “clicks” on exam. A majority of newborn “clunks” resolve by 2 weeks of age. So do NOT obtain any imaging at the time of birth. ALL patients with an unequivocal Barlow or Ortolani maneuver (meaning there’s no question in your mind on exam), limited hip abduction, or asymmetric hip abduction after 1 month should be referred to an orthopedist for evaluation. For children 6 weeks-4 months of age, ultrasound should be used. After 4 months of age, hip x-rays should be used. Treatment of DDH requires a Pavlik harness.PEARL: Consider imaging before 6 months of age for any male or female infant with normal findings on physical exam, but any of the following risk factors. - Breech presentation in the third trimester
- Positive family history
- History of previous clinical instability
- Parental concern
- History of improper swaddling
- Suspicious or inconclusive physical examPEARL: The age range to use ultrasound for diagnosis is 6 weeks to 6 months. Radiographs can be used after 4 months of age. Radiographs are preferred after 4 months due to the lower rate of false positives compared to ultrasound. NEVER image before 2 weeks of age. For a child with no clinical signs of DDH on exam but with a NEED for evaluation based on high risk factors, you can ultrasound at 6 weeks or obtain radiographs at 4 months of age. When it comes to the Barlow and Ortolani signs, if EITHER of them are positive, send for imaging as soon as possible (after 2 weeks of age)! ALL children should be “screened” periodically at the well-child visits by EXAM! Meaning, if you’re asked if you should “screen” a child for DDH at the 2-month visit, the answer is always going to be YES. Lastly, if you encounter an asymptomatic child that was supposed to get imaging (e.g., a breech baby) but never did, and the patient is now 5 or 6 months old, GET IMAGING even if the exam is normal!
https://pediatrics.aappublications.org/content/pediatrics/138/6/e20163107.full.pdf
https://www.aappublications.org/news/2016/11/21/DDH112116
https://www.aafp.org/afp/2017/0801/p196.html
– under CONTACT SPORTS PARTICIPATION – the paragraph reads ” Contact sports participation should be avoided in children with a SINGLE KIDNEY…” the following sentence then contradicts this and says that ” Those with a SINGLE KIDNEY…can participate.” I'm guessing the single kidney reference from the 1st sentence was wrong and should be removed? Please clarify as this point is very confusing.
- You are correct. We’ve updated the section.
- CONTACT SPORTS PARTICIPATION
Contact sports participation should be avoided in children with a single kidney, those with hepatosplenomegaly, and those who have had repeated concussions. Those with a single eye or single testicle can participate given proper protection of the remaining organ. A single ovary is not a contraindication to contact sports, though the issue is somewhat controversial (thus probably won’t be tested!).
==========================================
RHEUMATOLOGY
No Corrections! But the 2020 Pediatrics Board Review Study Guides May Have New Content (Or Corrections).
==========================================
PULMONOLOGY
No Corrections! But the 2020 Pediatrics Board Review Study Guides May Have New Content (Or Corrections).
==========================================
PSYCHIATRY AND SOME SOCIAL ISSUES
On page 409, it says for ADHD that symptoms need to be present prior to 7 years old. This is incorrect, according to the DSM 5 the symptoms need to be present before 12 years old.
- You are correct. See the updated section below.
- ATTENTION DEFICIT DISORDER (AKA ADD, ADHD, and ATTENTION DEFICIT HYPERACTIVE DISORDER)
Impulsive + Inattentive + Disorganized thoughts in a child = Attention deficit disorder (AKA ADD and ADHD). This must be DIAGNOSED AFTER 6 years of age, but symptoms must be PRESENT prior to 12 years of age. ADD is more common in boys than in girls. Fifty percent persist into adulthood, especially the inattentive/disorganized part. Sugar doesn’t exacerbate it. The best treatment is pharmacologic + “other” interventions (psych referral).
PEARLS: If a child was started on a stimulant medication and now pays more attention, that does not diagnose ADD. Before making the diagnosis, make sure lead poisoning, iron deficiency, vision problems, hearing problems, thyroid disorders, sedating medications (antihistamines, seizure medications), CNS infection, and CNS trauma have been ruled out. Other conditions to consider include hay fever, Klinefelter Syndrome, absence seizures, maternal drug/alcohol abuse, patient drug/alcohol abuse, and depression.
Is the screen time recommendations less than 30 min or 2 hours?
- This area is evolving. See updated material below.
- IMPACT OF MEDIA ON CHILDREN
Watching too much TV increases aggressive behavior and has a true influence on children’s diets due to advertising. TV also seems to obscure reality, as well as increase a sedentary lifestyle. Many children watch > 25 hours of TV per week. The most recent recommendations include:
- < 18 months, avoid TV/screen time except for video chatting
- 18-24 months, < 1 hour of TV/screen time with adult supervision
- 2-5 years old, up to 1 hour of high-quality TV/screen time with adult supervision
- Beyond that, a customized plan may be needed based on the family’s schedule and what type of media is being used. Use apps for learning but don’t use media as a pacifier. Have tech free zones.
TOOL: http://HealthyChildren.org/MediaUsePlan
==========================================
ETHICS
No Corrections! But the 2020 Pediatrics Board Review Study Guides May Have New Content (Or Corrections).
==========================================
PATIENT SAFETY AND QUALITY IMPROVEMENT
No Corrections! But the 2020 Pediatrics Board Review Study Guides May Have New Content (Or Corrections).
==========================================
PEDIATRIC LAB VALUES
DIRECT BILIRUBIN (AKA CONJUGATED BILIRUBIN)
This is defined as having a direct bilirubin level that is > 2 mg/dL, or a level that is > 20% of the total bilirubin (even in a newborn). Most common newborn jaundice issues are due to an indirect hyperbilirubinemia.
****PRIOR ADDITIONS MENTION 0.6, THIS STATES 2MG/DL… My understanding is that it should be > 0.1mg/dL
Below is what I have based on my research – please clarify!!
– If the infant has unconjugated hyperbilirubinemia (>2 mg/dL [34.2 micromol/L] at two weeks of age), this is often caused by breast milk jaundice, but other causes also should be considered, particularly if the total bilirubin is markedly elevated
– If the infant has conjugated hyperbilirubinemia, causes of cholestatic jaundice should be investigated promptly. Conjugated hyperbilirubinemia is defined as a serum conjugated bilirubin concentration greater than 1.0 mg/dL (17.1 micromol/L) if the total bilirubin is <5.0 mg/dL (85.5 micromol/L) or greater than 20 percent of the total bilirubin if the total bilirubin is >5.0 mg/dL (85.5 micromol/L)
- Please note that the video states 0.6 and is incorrect. The current edition of the online and hardcopy PBR Core Study Guide are correct. This link may help to show that the AAP agrees with what we’ve written about a direct/conjugated hyperbilirubinemia being defined as greater than 2 mg/dL or > 20% of the total bilirubin. Your finding of > 1 mg/dL looks like it’s from UpToDate and you’ll have to decide if you want to side with the AAP or UpToDate.
- The Direct hyperbilirubinemias are the more Dangerous ones.
- The indirect hyperbilirubinemias can have much higher levels in the neonatal period, and we’ll refer you to the Neonatology chapter for a review of our cut offs and mnemonics to help you remember the guidelines for when to start phototherapy.
==========================================
PEDIATRIC VITAL SIGNS
No Corrections! But the 2020 Pediatrics Board Review Study Guides May Have New Content (Or Corrections).
==========================================
STRONG WORK EVERYONE!
THANK YOU SO MUCH FOR CALLING US OUT!
NOW LET’S GO OVER THE CLARIFICATION REQUESTS!
Again… we’ve tried to be as concise as we can because we know your time is short.
This section is going to cover CLARIFICATION REQUESTS from members and anything that we happened to find on our own that we felt might warrant a clearer explanation.
“Do you think we should study tympanograms?”
> Please avoid straying too far off of the PROVEN PBR PATH right now. It’s possible you’ll get ONE question on this. That’s too low yield for you to pursue studying now. Focus on the rest of PBR, which covers ALL of the very LOW HANGING AND HIGH-YIELD FRUIT!… AND SO MUCH MORE!
“I've seen a couple of practice questions about XXXXXXX and about XXXXXXX. I think you should consider maybe including these topics in the PBR.”
Thanks so much for ALL of your submissions, but 9 out of 10 times we will not tend up adding new topics to the PBR. Trust me when I say that it’s VERY possible to pass the exam with a first edition of the PBR from 2011. PBR will NEVER be a mini-Nelsons. Meaning, it’ll NEVER be a book where you can turn to for every pediatric diagnosis known to man. The PBR Certification System was not create to help you become the most well-rounded and knowledgeable pediatrician in the world. It is meant to give you MORE than what you need to pass the pediatrics boards with a score that is ABOVE the national mean! Know it inside and out… and ignore everything else. Otherwise, you’ll find that there’s ALWAYS going to be more information that you could potentially chase. It’ll lead you down a rabbit hole… or the BLACK HOLE of Google Search.
==========================================
ADOLESCENT MEDICINE
In your 2018 video, it says ” teach adolescent girls breast exams” yet in the 2019 book it says it's no longer indicated.
- The 2019 book is the most updated resource we have.
Does menses start at SMR 3 OR 4, or SMR 4-5? I did a medstudy question that stated it's SMR 4-5… yet in PBR (page 56) it says SMR 3-4.
- PBR is correct here. There is definitely a range here, so the boards will not ask for 3 vs. 4. Instead, they’ll give you other things to think about to see if the child is physiologically developing normally. Based on what has, or has not, happened you may be expected to make a diagnosis or suggest a workup.
- “Menarche typically occurs within 2–3 years after thelarche (breast budding), at Tanner stage IV breast development, and is rare before Tanner stage III development. By age 15 years, 98% of females will have had menarche (2). An evaluation for primary amenorrhea should be considered for any adolescent who has not reached menarche by age 15 years or has not done so within 3 years of thelarche. Lack of breast development by age 13 years also should be evaluated.”
- Click Here for a Reference
How in depth should we know about menorrhagia? The book has a brief blurb:
MENORRHAGIA AND AMENORRHEA
During the first two years of menstruation, infrequent menstrual cycles, or cycles lasting 2–3 days is OKAY. Menstrual period lasting > 10 days are abnormal and require a menorrhagia workup.
I know I shouldn't… but I went to uptodate to look up the work-up of menorrhagia… and came across this:
Heavy menstrual bleeding — Based upon current terminology, regular bleeding that is heavy or prolonged (referred to as heavy menstrual bleeding) refers only to cyclic (ovulatory) menses. The term heavy menstrual bleeding (HMB) was introduced as part of the PALM-COEIN (polyp, adenomyosis, leiomyoma, malignancy and hyperplasia, coagulopathy, ovulatory dysfunction, endometrial, iatrogenic, and not yet classified) classification system for AUB [3]. This replaces the term menorrhagia, which was previously used to describe heavy or prolonged uterine bleeding. Menorrhagia is a less precise word because it does not differentiate between volume and duration of bleeding or between cyclic and anovulatory bleeding
Which led to more questions, i.e. will the test describe menorrhagia, or should I also know it has “heavy menstrual bleeding”… ?
Thanks for the question. Here are some thoughts from our adolescent medicine specialist.
- “Primary amenorrhea” is when 2 years have passed after breast development begins. If breast development started at 8 years of age and now the patient is now 13 and still hasn’t had menses, that’s not normal.
- “Menorrhagia” is about signs of high volume (e.g., 8 pads or 4-5 tampons per day).
- “Menometrorrhagia” is about the duration. If > 7 days, that’s abnormal. Every 21-35 days.
Per PBR: “Menstrual period lasting > 10 days are abnormal and require a menorrhagia workup.” What consists of menorrhagia work up?
- Same work-up as dysfunctional uterine bleeding with pregnancy being the most common cause. See the following link for more details, but you should check a CBC and TIBC for anemia, coagulation factors, CMP, TSH, and prolactin levels.
- https://emedicine.medscape.com/article/255540-workup
Book states:
Do a workup for primary amenorrhea if the patient has not had menses in the presence of ANY of the following:
It’s been 2 years since puberty ended. For example, if puberty started at age 8 and finished at age 11, there is no need to do a workup until at least age 13.
My question is: What are signs we should look for that puberty has ended?
- The presence of MENSES and SMR 5 breasts (round appearance) and pubic hair.
When would we use growth hormone?
- Uses of growth hormone in pediatrics is typically limited to growth hormone deficiency, and in some specific syndromes such as Prader Willi (beyond the scope of the board exam).
==========================================
ENDOCRINOLOGY
Why does renal disease cause a high phos and normal Ca? (this confused me bc it is the opposite in familial hypophosphatemic rickets which is a renal disorder) p. 78 of book
- This is because of differing physiology. On the renal front, it’s very complicated and involves a dance between the lack of excretion of phosphorus from the kidneys, the role of PTH on the bones and intestines, the lack of calcitriol due to dysfunctional kidneys. Normal working kidneyscan remove extra phosphorus in your blood. When you have chronic kidney disease (CKD), your kidneys cannot remove phosphorus very well. High phosphorus levels can cause damage to your body. Extra phosphorus causes body changes that pull calcium out of your bones, making them weak. Thus, it results in high phos and normal to high Ca in blood
Why does ADH go up in Addison disease…. it confused me bc wouldn't that cause [Na] to go down and you already have hyponatremia in Addison disease due to aldosterone deficiency? p.79
- Sodium is what’s needed to expand volume, but if you can’t do that then your body tries to do whatever it can to retain fluid. These kids are VERY hypovolemic because of the lack of aldosterone when they are untreated. The increase in ADH results in decreased urine output in an effort to preserve enough volume to survive. As mentioned in the Core Study Guide, “Think of the rise in ADH levels as an appropriate effort to retain water due to insufficient mineralocorticoid (aldosterone).”
What’s the preferred treatment for Graves’ disease in pregnant women? Isn’t it Methimazole > PTU? I’m confused b/c p. 74 (2019 book) says PTU is toxic but then on p. 75, it says “PTU is okay to give during Pregnancy”. Please clarify anyone!
- Good question. The preferred treatment is Methimazole. As mentioned, though, PTU is “Potentially Toxic, Ugh!” So, while it can be used in pregnancy if needed, you have to monitor for toxicities.
Why isn’t fludrocortisone part of the treatment for adrenal crisis but is treatment for primary adrenal insufficiency? (P.80 of 2019 book)
- It depends on the underlying cause of the adrenal crisis (primary vs. secondary), but the mineralocorticoid is not emergent for adrenal crisis in secondary adrenal insufficiency. Administering a supraphysiologic/stress dose of glucocorticoid (IV hydrocortisone) is the only definitive therapy for adrenal crisis with IV SALIVE AND IV GLUCOSE as written in the book. Fludrocortisone, a mineralocorticoid, may also be given after the initial resuscitation.
==========================================
OB/GYN AND SOME STDs
Question regarding this pearl: PEARL: In general, when you think the diagnosis is due to a Chlamydia species, choose doxycycline if the child is > 8 years of age, or choose a macrolide (usually erythromycin). Also, this is an intracellular organism. Look for the phrase “intracytoplasmic inclusions.” In practice, we often just use azithro x 1, is the exam answer more commonly doxy, is that why this pearl is here?
- Azithromycin x 1 day OR Doxycycline x 7 days are equally effective. Doxycycline has concerns for teeth staining, so that’s why we try to avoid it when possible until a child is at least 8 years of age.
The latest pbr book states regarding ASCUS “Pap smears are being performed less frequently in young adults. If a pap reveals ASCUS in a woman under age 24, then repeat a PAP smear in 1 year. If the second PAP smear also shows ASCUS, then consider a colposcopy.”
But the latest video on PBR states, if +ASCUS – do colposcopy in 6 months. Can you clarify what we should memorize in this case?
- The book is correct and more up to date.
On page 85, you discuss contraindications to OCPs: migraine with aura is not listed and should be.
- You are correct! Based on limited data, there is a very small risk of ischemic stroke for anyone who suffers from migraines with auras. This is a relative contraindication. There are additional contraindications as well, but we’ve chosen to focus on a few of the ones that we think are more likely to be tested.
Would a history of DVT’s or clotting issues also be an absolute contraindication for OCP’s?
- This is complicated. For young, healthy females, the likely of DVT is low. So for the peds boards, this would not be the case. Regarding clotting disorders, the likelihood of 1 clotting disorder causing clots can be very different when compared to the likelihood of another clotting disorder. So it’s definitely a relative contraindication, but not an absolute. Keep in mind that different sources cite different absolute vs. relative contraindications.
==========================================
ALLERGY AND IMMUNOLOGY
Is a bone marrow transplant the correct treatment for Bruton's, SCIDs, and Wiscott-aldrich?
- The answer is YES. But, Dr. Kara Wada (allergist and immunologist) and Team PBR feel that you are unlikely to be tested on the ABP Initial Certification exam on how to cure these disorders. Dr. Wada feels that such question are likely only appropriate for allergy subspecialty boards. So, “yes, but that information is likely low yield.”
Are live vaccines contraindicated in SCID, Digeorge and Wiscott-aldrich?
- That is correct. Live vaccines tend to be contraindicated in most of the T-cell disorders.
With respect to skin rash developing 1-2 days after giving patient Penicillin/Amoxicillin (not uncommon complaint in clinic!), is this a contraindication to using Amoxicillin for patient's next Strep Throat or AOM?
- Unless the rash includes blistering and peeling of the skin, such rashes are usually related to the illness itself rather than penicillin or amoxicillin. Therefore, such a rash would not be a contraindication to future penicillin or amoxicillin use.
==========================================
CARDIOLOGY
Anybody have a simple way to remember heart murmurs?
- Hmm.. not so much. But here’s a chart below for review from the American College of Cardiology. Hope it helps!
[IMAGENEEDED] – 32
In Kawasaki's disease, what is the reason for providing 2nd dose of IVIG (for boards)?
- It’s controversial. Some people give steroids or other medications. General consensus is to try again if the first dose doesn’t work. Some institutions also use Rituximab. Given that it’s controversial, you shouldn’t be asked for the reason.
Do you use IVIG to prevent or treat aneurysms in Kawasaki's?
- It’s used to prevent the aneurysms. Once an aneurysm forms, you cannot give medication to make it go away.
How do you tell the difference between constrictive pericarditis vs restrictive cardiomyopathy?
- The chart below illustrates the difference between restrictive and constrictive pericarditis from American College of Cardiology. For the residents, the most important and easy thing to remember is that there is significant bilateral atrial enlargement (huge atria – mostly bigger than ventricles) which is generally not seen with constrictive pericarditis.[IMAGENEEDED] – 33
Do you have a simple way to remember AVRT? Thank you again for all of your help and as always.
- I am not sure which part you need help remembering, or differentiating from something else, but we can provide some basic concepts/points which can help you remember and answer any questions on the topic.
- AVRT – Atrio-ventricular re-entrant tachycardia it a type of re-entrant tachycardia:
- All en-entrant tachycardia are of sudden onset.
- They respond to vagal maneuvers and adenosine (adenosine should not be given with wide complex tachycardia or atrial fibrillation).
- Long term treatment with beta-blockers or EP ablation.
- All AV re-entrant tachycardia have accessory/additional pathway. If the pathway lies within/or proximity to the AV node itself, it is call AVNRT (AV nodal re-entrant tachycardia).
Why is the test of choice a CXR rather than an ECHO. CXR will not alert to tamponade physiology.
- It depends on the scenario and circumstances. If you are sitting in ED and suspect a pericardial effusion, the CXR is the easiest and fastest test to perform which will show cardiomegaly (and you can call a cardiologist for and echo). As you are rightly thinking, ECHO is the gold standard and will also delineate the tamponade physiology.
I'm getting confused with murmur for TOF and PS… So, in TOF, you get PS murmur… which I thought is a wide split S2, like RBBB.
But in the notes, it says “PE: PS murmur (harsh LUSB murmur, a single s2, a single S1, and possibly a click). Note that the P2 component is SO soft that it simply sounds like a single S2.”… so is it a single S2, or wide split S2? I feel like I'm missing something key!!
- The characteristic of murmur depends upon the severity of stenosis and condition of pulmonary valve. In general, pulmonary stenosis (in TOF or without it) causes delayed P2 component (wide split) with a click. But in TOF, mostly the stenosis is at the level of RVOT (right ventricular outflow tract) muscle bundle and pulmonary valve itself might be dysplastic leading to loud ejection systolic murmur (similar to PS murmur but originating from RVOT) with soft P2 sounding like single S2.
Question about ductal dependent lesions in CHD. On page 124 under PGE – there is a discussion on ductal dependent lesions. “Prostaglandin (also known as PGE1 or alprostadil) is the medication given to keep the ductus arteriosus open. This may be needed when faced with a left-sided obstructive lesion (e.g., coarctation of the aorta, critical aortic stenosis, hypoplastic left heart) or a right-sided obstructive lesion (e.g., tricuspid atresia, pulmonary atresia, TOF with pulmonary stenosis).” Is this list inclusive?
Would TGA/TOGA be considered a ductal dependent lesion as well since treatment is creating VSD and PDA (text states mixing at PDA not as helpful as ASD creation)? My goal was creating list of all CHD that are ductal dependent.
- Congenital heart disease is very complex, and many times patients have a mixed lesion. For example, a DORV (double outlet right ventricle) patients might be ductal dependent or independent depending upon the associated lesions (like, pulmonary stenosis/aortic stenosis). In general, PGE is indicated if there is any sign of insufficient pulmonary or systemic blood flow. Again, in TGA (in general) the mixing is the best at the ASD level, but sometime PDA level shunt is also needed. I think for boards, the focus should be at what the question is asking. If there are signs of insufficient systemic (pallor, decreased peripheral pulses) or pulmonary circulation (oligemia with cyanosis) then PGE is indicated.
My question is regarding prophylaxis in repaired cyanotic CHD with prosthetic material. In PBR: “REPAIRED CYANOTIC CHD with prosthetic material Prophylaxis for 6 months after surgery. Unless prosthetic VALVE material was used, lifelong prophylaxis is NOT indicated”. In OVC he mentioned “(for prosthetic material used in vsd)… Residual leak causes epithelization so give lifelong prophylaxis.” I am wondering if prosthetic material was used, not on the valve, but for instance on the VSD, then according to OVC we give lifelong ppx, but in the book it implies we only give it in the first 6 months?
- Yes, the book is correct. Repaired CHD (e.g. VSD) with residual defects at the site or adjacent to the site of a prosthetic patch or prosthetic device (which inhibits endothelialization) requires lifelong antibiotic prophylaxis.
- https://emedicine.medscape.com/article/1672902-overview
==========================================
DERMATOLOGY
p.142 and p.395 – under NEONATAL LUPUS; please clarify the diagnosis of anti-RO and anti-LA antibodies – is it from mother or baby? According to the National Organization for Rare Disorders, diagnosis should be made by maternal antibodies only; since their crossover is what causes the baby's symptoms. Please mention this specific detail so that we know to check MATERNAL anti Ro/La and not neonatal.
- Check maternal anti-Ro/La antibodies. Any pregnant woman who has anti-Ro/La antibodies should have weekly fetal echocardiograms beginning at 16 weeks' gestation to look for possible signs of congenital heart block. Thanks for the clarification request. We’re updating our Core Study Guide topic for 2020.
- (DOUBLE TAKE) NEONATAL LUPUS
The baby does NOT have lupus. Neonatal lupus occurs in children of mothers with SLE due to fetal exposure to maternal SLE-related antibodies. It is rare. Findings may include increased LFTs, petechiae, rash, scaling, thrombocytopenia, third degree AV heart block with bradycardia, or hydrops fetalis (fluid accumulation in two or more fetal compartments usually due to heart failure). Diagnose by sending maternal Anti-Ro or anti-La antibodies (AKA anti-SS-A or SS-B).
IMAGE: www.pbrlinks.com/NEONATALLUPUS1
Please clarify if an infant found to have HSV gingivostomatitis (who is tolerating PO) still requires IV acyclovir.. ? The video mentioned around 1:07:02 that babies need IV acyclovir even in hsv gingivostomatitis, but in clinical practice I thought we treat HSV gingivostomatitis with supportive care, including babies.
- You are correct, treat immunocompetent hosts with supportive cares, but immunocompromised hosts with IV acyclovir. We will check the video and make sure that fact is clearly stated. As for a sneak peek at the 2020 Pediatrics Board Review Core Study Guide…
- (DOUBLE TAKE) HERPES SIMPLEX VIRUS GINGIVOSTOMATITIS
Herpes simplex virus gingivostomatitis presents with oral and perioral/vermillion border lesions/vesicles. Gingiva is friable and malodorous. There is associated lymphadenopathy. Usually caused by HSV-1. Can treat with oral acyclovir, but there is limited data supporting this in children. Treat immunocompromised hosts with IV acyclovir.
IMAGE: www.pbrlinks.com/HSVSTOMATITIS1
Can you go over why in cellulitis, cefazolin is the best choice… as opposed to say, keflex or augmentin? The book mentions “For treatment, start with Cefazolin as your first line agent.” Is that just the antibiotic that's tested more?
- It depends on if you are treating inpatient (IV) or outpatient (PO), the local Staph aureus susceptibility data and the risk for MRSA. Choose as narrow spectrum antibiotic as possible. Cefazolin (Ancef) is a 1st generation cephalosporin and is only available IV, so must be used in the inpatient setting. It has good coverage for Staph aureus (MSSA) and Strep pyogenes (Group A Strep) and other strains of streptococcus such as group B Streptococcus (GBS). Cephalexin (Keflex) and Amoxicillin-Clavulanic Acid (Augmentin) also have good staph and strep coverage and are available in PO form.
- CELLULITIS
Cellulitis is defined as a well-demarcated area of erythema, edema, and induration secondary to an infection. It may be associated with bullae. For treatment, start with a 1st generation cephalosporin such as Cefazolin or Cephalexin as your first line agent.
Wanted to clarify that in setting of rhus dermatitis, oral steroids are not always indicated. Oral steroids are often used to treat rhus dermatitis when there are large reactions that lead to swelling around the eyes or genitals. You can give topical steroids if the involvement is mild. Right?
- No, oral steroids are only indicated for severe cases that involve swelling around the eyes or genitals.
- Rhus dermatitis typically presents as linear streaks of vesicles in areas where the plant comes into contact with the skin. It is a T-cell mediated Type IV hypersensitivity reaction caused by the exposure of the skin to poison ivy, poison sumac, or poison oak antigens. The rash is very itchy, and the treatment is focused at reducing the itch and discomfort associated with the rash.
- Treatment of mild to moderate cases consists of cool compresses, as well as medium-to-high dose topical corticosteroids. An oral antihistamine is often also used to decrease the pruritus.
- Treat severe cases with oral steroids if the rash is around the eyes or genitals and involves a large surface area of the skin. Give oral steroids for at least 2 weeks as there can be a rebound phase if treatment is too short.
- Eliminate any further exposure to the antigen by washing the skin and fingernails with soap and water to remove any remaining antigen. The fluid from the ruptured vesicles does not cause a spread of the dermatitis, therefore there is no need to cover the rash. Clothes should also be washed, as any remaining antigen could lead to the development of new areas of dermatitis.
Thanks for submitting the question. We’ll make some modifications in this topic for 2020.
- ALLERGIC CONTACT DERMATITIS, A TYPE IV HYPERSENSITIVITY SKIN RASH
Allergic contact dermatitis is a Type IV hypersensitivity skin rash that requires a prior exposure, and tends to be pruritic. See if the location of the rash is in an area where a nickel-containing belt buckle, earring, necklace, or other jewelry could have been. A rash may present even after years of wearing the irritant. The rash from nickel exposure is more erythematous and can become lichenified. The classic example of Type IV reactions is the rash of poison ivy, or other “leaves of 3” (including poison oak and poison sumac). Regarding a contact dermatitis from these plants, it will not spread once the affected area is washed with soap and water. The fluid from within the vesicles cannot spread the rash. This reaction is a Type IV Cell Mediated Hypersensitivity Reaction, and is called a Rhus reaction (from the old genus name of poison ivy, Rhus radicans). The rash is vesicular and may be in a linear configuration (where the leaves rubbed across the skin).
* PEARL: First exposure may take 1 week to develop the rash as helper T cells proliferate and “remember” the agent. After that, the rash may develop within hours of exposure. “No wonder I had to go through the 2-step PPD before starting as an attending!”
* PEARL: REMINDERS: A PPD and the skin testing of Candida, Mumps, and Tetanus are all Type IV reactions.
* MNEMONICS:
“LEAVES OF THREE, LET THEM BE!”
Type IV reaction: I + V = the Roman numeral IV = 4, and the 4th letter in the alphabet is D = DELAYED. I + V also should you remind you of poison IVy.
[IMAGENEEDED] – 38
Ref: Wikipedia.com
p.145 and p.374 – PHACES Syndrome – under the acronym “H,” it says that hemangioma can be associated with strokes. However, just below that, the acronym “A” is for arterial cerebrovascular anomaly. Therefore I think the last line from the “H” acronym regarding association with strokes needs to actually be moved to the following line from the “A” acronym, since CVAs have a known relationship with stroke, but hemangioma and stroke association makes no sense. Please clarify.
- Yes, you are correct. This will be updated as shown below. https://pediatrics.aappublications.org/content/117/3/959
- PHACES SYNDROME
A diagnosis of PHACES syndrome requires a large hemangioma in the face/neck area PLUS one of the following defects:
* Posterior fossa malformation (DANDY WALKER)
* Hemangioma. Often in the distribution of the Facial Nerve. Look for a large segmental hemangioma on the FACE. Segmental refers to what looks like a nerve distribution (segmented by normal skin in between).
* Arterial cerebrovascular anomaly. This can be associated with STROKES.
* Cardiac anomalies: Especially COARCTATION OF THE AORTA
* Eye anomalies: MICROPHTHALMIA, STRABISMUS
* Sternal defect
* IMAGE: www.pbrlinks.com/PHACES1
Can you summarize the use of the Tzanck stain?
- Simple test that looks at single cells and is mainly used to rapidly detect herpes infection or distinguish SJS/TEN from staph scalded skin syndrome. https://www.dermnetnz.org/topics/tzanck-smear/
==========================================
NEONATOLOGY
p.162: regarding WHOLE MILK consumption between 1-2 years old- can you please write Bullet Point 2 with more clarification? Do you mean to say that: whole milk is recommended for all healthy children with no risk factors; 2% milk is recommended for at-risk children (overweight or obese, +FHx of obesity or cardiovascular disease)?
Updated section below.
WHOLE MILK
- * Whole milk should NOT be given to babies until they are 1 year of age. It can cause anemia, electrolyte abnormalities, such as hypocalcemia, and renal damage.
- * Give whole milk from 1−2 years of age. The fat content helps with nervous system development. However, 2% milk is recommended for children who are at risk of being overweight or have a family history of obesity or cardiovascular disease.
- * After 2 years of age, CHANGE to 1% or skim milk in order to LIMIT the fat content.
If fluid in the horizontal fissure is noted in a newborn with tachypnea, pick transient tachypnea of newborn. Can't it also be neonatal PNA? You can have fluid in horizontal fissure for PNA… I'm just uncertain why fluid in horizontal fissure should reflexively make me think TTN, appreciate the teaching.
- The cause of TTN is thought to be secondary to delayed resorption of fetal lung fluid. The fluid fills air spaces and perivascular tissues and the interlobar fissures and is eventually cleared by the lymphatic system.
- https://www.uptodate.com/contents/transient-tachypnea-of-the-newborn
==========================================
DEVELOPMENTAL MILESTONES
p.175 – GROSS MOTOR section for the 6 m/o developmental milestones chart: 2nd sentences says “Sits using hand support.” However, the 1st MNEMONIC, 2nd sentence reads as “If a Six-month old is strong and coordinated enough to SIT WITHOUT SUPPORT, he can also roll in two different directions.” I think you meant to say “sit with support” in the mnemonic, correct? This would mean the mnemonic may need to be changed – sorry Ashish! (your 9 m/o developmental chart reports “sits without support” so I'm guessing the mnemonic was a typo). I also cross checked this specific milestone with other sources which all state “sit with support” for a 6 m/o.
- We get a lot of these questions every year. There’s plenty of variability out there between different sources.
- The mnemonic and the book are correct. According to the Denver II, a child can sit without support between 5-7 months with 90% sitting without support at 7 months. Only about 50% of children at 6 months can sit without support, thus the mnemonic saying…IF A SIX-MONTH OLD CAN SIT WITHOUT SUPPORT (Which 50% can do at that age), then they can roll in both directions. IF A SIX-MONTH OLD CANNOT SIT WITHOUT SUPPORT (Which 50% cannot do at that age, then they cannot roll in both directions).
p. 181 – LANGUAGE section for the 3 y/o developmental milestones chart: 3rd sentence says, “Uses plurals.” I think you meant to say, “Uses pronouns.” Please correct.
- The book is correct. A 3-year-old uses plurals AND uses pronouns. Our editor, Dr. John Cole, strongly encourages you to use the mnemonic stories. He said that they are very helpful. He even started dreaming about Crayola!
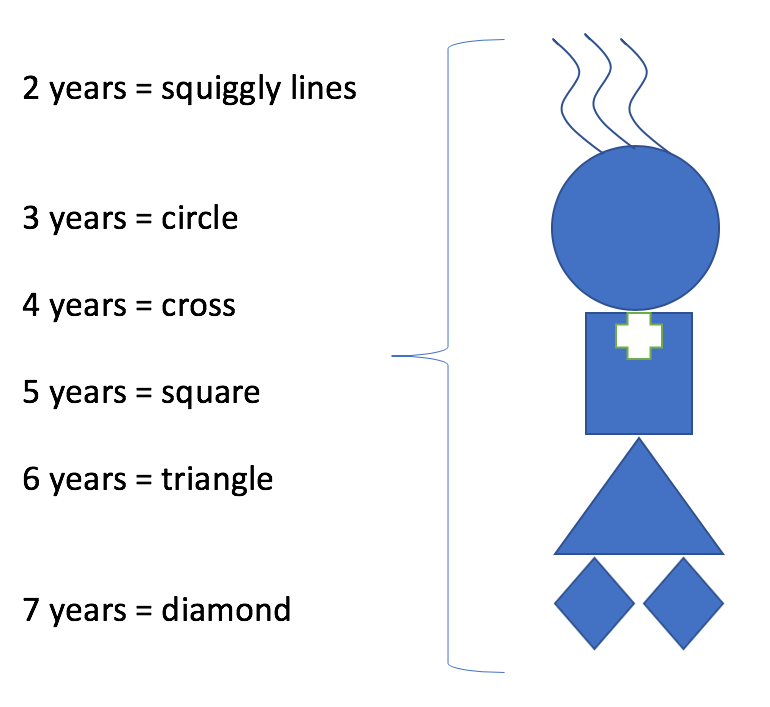
The book pge 172 a 5 year old can draw a square, 6 year old triangle and 7 year old diamond. I had questions in AAP and medstudy where this is incorrect and a 5 year old can draw a triangle and a 6 year old can draw a diamond. Could you please clarify which is the correct one. Thank you
- Again, there’s a lot of variability out there between different sources. If you look at the DENVER II, you’ll see that the age ranges for the circle, cross and square actually line up with PBR fairly nicely. And if you do an online search for milestones, you’ll see that they are extremely variable depending on where you go. Our chapter in PBR, as is, has served the author (Ashish), editor (John), and thousands of other PBR alumni VERY well. Their scores in that section have SKYROCKETED. My recommendation is that you use ONE resource for this section (PBR’s) and know it inside and out! Last, PUT NELSON’S DOWN! Do not use it to study. Bad, bad, bad idea. It’s overwhelming and not high-yield. My hope is that you used it for just a few minutes as a reference.
- The head is the circle (3), squiggly lines for hair on top of head (2), necklace is a cross (4), body is a square (5), dress is a triangle (6) and the legs are diamonds (7).
The exam has multiple question regarding bilingual kids and what is expected for milestones. for language bilingual kids should be the same as monolingual?
- Instead of focusing on the “lower” milestones, pick an age that is consistent with the more advanced milestones.
==========================================
EMERGENCY MEDICINE AND TOXICOLOGY
Button battery ingestion- Don't we have to remove it, irrespective of where it is but “core content study book” says if the battery has passed beyond the esophagus, leave it because it will pass without problems. Remove it only if in the esophagus?
- Book is right. Only remove if stuck and not passing.
The book on p.188 says bowel sounds go up in sympathomimetics, but video says bowel sounds go down…. which one is correct?
- The book is correct.
On page 189, the section on ethanol, it states that it has a positive anion gap, it should say positive osmolar gap. Ethanol does not lead to an anion gap metabolic acidosis.
- Ethanol (ETOH) can lead to an anion gap. But you are correct in saying that an osmolar gap is also present. We discuss this in our PEARL/SHORTCUT from the ISOPROPYL ALCOHOL section.
- In going through this, we also realized that we accidentally used “ETOH” instead of the word “alcohol” in the ISOPROPYL ALCOHOL section on page 190 in the first PEARL. We’ve corrected that error and are including this question and the answers in both the Corrections section and the Clarifications section of this guide. Thank you! Updated topic below.
- ISOPROPYL ALCOHOL
PEARL: There is NO anion gap. If alcohol is positive and there is NO anion gap, choose ISOPROPYL ALCOHOL poisoning. If an anion gap is PRESENT, choose ETHANOL, METHANOL, or ETHYLENE GLYCOL. This is not intuitive, given the presence of ketones, but knowing this could be key.
The antidote for anti-cholinergic Toxidrome is to give physostigmine. Why wasn't that mentioned as the treatment?
- Good idea! We’re updating our ANTICHOLINERGICS section.
- ANTICHOLINERGICS
Use of anticholinergics may result in fever, blurred vision, DRY MOUTH/EYES, hyperthermia, psychosis, DECREASED BOWEL SOUNDS/MOTILITY, URINARY RETENTION, and tachycardia. These patients also have MYDRIASIS. Medications with anticholinergic effects include diphenhydramine, ATROPINE, pralido- xime, TRICYCLIC ACIDS (TCAs), and JIMSON WEED. Treat with CHARCOAL. For severe cases with central and peripheral signs and symptoms of anticholinergic poisoning, treat with physostigmine.
PEARL: Due to decreased bowel motility, it is OKAY to give charcoal even after 60 minutes for an anticholinergic ingestion! For other medications, though, 60 minutes is the limit.
MNEMONICS: HOT as a hare, BLIND as a bat, DRY as a bone, RED as a beet, MAD as a hatter while the BOWEL and BLADDER lose their tone, and the HEART runs alone. In AAA$, the third A is for Anticholiner- gics or Atropine. For Jimson WEED, imagine Harold and Kumar smoking “WEED” at a White Castle® that has plenty of food, but NO DRINKS (DRY mouth, slow passage of foods in the GI tract because the food is “dry”).
MUDPILES is for anion gap metabolic acidosis. Is CUTE DIMPLES for Osmolar Gap? Or just another mnemonic for anion gap? Did you mean to add something about the difference between AG & OG? I just thought it seemed like something was missing. Also, I think toluene is a NON-AG metabolic acidosis.
- Both mnemonics are for a high anion gap metabolic acidosis. Toluene can be the cause of either a normal or high-anion gap metabolic acidosis. Teophylline is another cause of high anion gap metabolic acidosis if you would like to replace the “T” with that.
==========================================
VITAMIN AND NUTRITIONAL DISORDERS
Why is B12 supplementation given by IM rather than PO?
- The dose of B12 that needs to be given is quite high, and the PO absorption is not good enough to allow a single administration. The same goes for intranasal administration. Therefore, it’s given intramuscularly for a “one and done” option.
p.207 and p. 269 – section on B12 DEFICIENCY – The order of the material in the following line is incorrect: “Look for intrinsic factor deficiency (pernicious anemia) or an inability to absorb B 12 due to gastric surgery (diagnosed with autoantibodes to intrinsic factor).” That last parenthesis about autoantibodies is specifically associated with pernicious anemia; not gastric surgery. Please relocate this part to the initial parenthesis with pernicious anemia to avoid confusion; you can instead add a parenthesis after gastric surgery to say something like “(due to loss of gastric parietal cells responsible for intrinsic factor production)” – otherwise everyone would think gastric surgery leads to autoantibody formation to intrinsic factor lol. Sorry, Ashish..I”m being nit picky here – but it took me awhile to understand in this paragraph what was trying to be said lol…
- I see your point here. We will switch the parenthesis as shown below.
- Look for INTRINSIC FACTOR DEFICIENCY (Pernicious Anemia, diagnosed with autoantibodies to intrinsic factor) or an inability to absorb B12 due to gastric surgery.
- (DOUBLE TAKE) B12 DEFICIENCY (AKA CYANOCOBALAMIN DEFICIENCY)
Cyanocobalamin (Vitamin B12) deficiency can present as a macrocytic anemia in a patient with neurologic issues (paresthesias, ataxia, and decreased reflexes). B12 deficiency can also result in neural tube defects (such as spina bifida) in the unborn fetus if a pregnant woman is deficient. Common causes of B12 deficiency include diet (VEGANS) and an inability to absorb B12. Look for INTRINSIC FACTOR DEFICIENCY (Pernicious Anemia, diagnosed with autoantibodies to intrinsic factor) or an inability to absorb B12 due to gastric surgery. B12 is absorbed in the terminal ileum, which means it may be lacking in patients with Short Bowel Syndrome, bacterial overgrowth, or Inflammatory Bowel Disease (IBD). Treat with IM B12 injections.
PEARLS: B12 will likely be used on the exam, but KNOW that B12 = CYANOCOBALAMIN. In a B12-deficient patient, if a macrocytic anemia is noted and mistakenly treated with folate supplements, the B12 deficiency will be MASKED as the megaloblastic anemia improves. This can eventually lead to irreversible neurologic damage.
==========================================
GASTROENTEROLOGY
Anytime barium swallow is the answer, I get it wrong. Can you please go over what we need to know with respect to barium swallow? For instance, a question in PREP 2015, Question 212. Test describes an infant who has GERD-like symptoms and wheezing, not improving with albuterol. Next best test? Barium swallow! (I picked allergy testing which was wrong).
- This can be confusing, so you have to know if they are asking about a modified barium swallow series or an upper GI barium. The upper GI series looks at the anatomy (hiatal hernia, malrotation, etc.). A modified barium swallow is used by the radiologist and the speech therapist to look for signs of aspiration. In the question you mentioned, the child has known GERD symptoms and has respiratory symptoms that are not responding to albuterol. Therefore, a modified barium swallow would be appropriate to see if the child is aspirating while during drinking, or while refluxing.
Is Gardners syndrome (page 238) a type of familial Adenomatous polyposis?
- In the GI OVC webinar we incorrectly stated that Gardners Syndrome is not related to Family Adenomatous Polyposis, but it is. The new version of the book will state that Garner syndrome is a subtype of familial adenomatous polyposis. The primary findings in Gardner syndrome (AKA Gardner’s syndrome) are the premalignant polyps throughout the intestines. Other findings include supernumerary teeth (extra teeth) and tumors in other parts of the body (especially benign bone tumors, called osteomas).
For H.pylori diagnosis on peds boards, is the first step to do a stool antigen or EGD?
- In practice, we do a stool antigen initially. For the boards, always do an EGD with biopsy.
For a child with physiologic reflux, would you choose thickening feeds or observation?
- If the child is thriving, then there is no need to have an intervention.
Can you go over Hepatitis B serology, specifically acute vs. chronic? I get confused with Anti HepB core presence in both. Will the IgM Anti Hep B core be present in acute?
[IMAGENEEDED] – 46
- See the above chart (https://pbrlinks.com/hepbserology) for reference. A positive anti-HBc IgM usually indicates a new acute infection and a positive anti-HBc IgG usually indicates a chronic infection.
Can you go over ERCP and MRCP and what we need to know for boards?
- They both look for biliary obstruction. MRCP is noninvasive but it’s also only diagnostic. ERCP is diagnostic but can also be therapeutic. If you do not suspect biliary obstruction, or if the suspicion is low based on your exam and lab findings, then MRCP is a good first step.
Can you clarify whether intussusception is 3mo to 3yo, or 3mo to 6yo? PBR states 6yo but other sources I read said 3yo. I want to make sure.
- Intussusception – typically 3 – 36 mo; most <24mo
Can you please clarify pyloric stenosis US diagnosis? On uptodate.com, it says “Criteria defining the upper limits of normal range from PMT 3 to 4 mm, PML 15 to 19 mm, and PD 10 to 14 mm”… I had a case the other day of it in the Peds ED, and the radiologist told me that they mainly look at the pyloric diameter to help guide them? Just want to know what I need to for the exam, if you say it's 14mm for PML and 4mm for PMT I'll memorize that, but wanted to clarify since when I told the radiologist my PBR knowledge…he said that's not what they go by, and they use PD more.
- May need to clarify with radiologist – depends on size of baby as well, whether they were preterm or not; PMT 3 – 4 mm, PML 15 – 19 mm and PD 10 – 14 mm are the upper limits of normal. In terms of which measurement – depends of radiologist: if clinical picture is suggestive of PS and measurement is suspicious Dx is likely PS.
==========================================
PHARMACOLOGY AND DRUG PEARLS
On p. 230 – under ISOTRETINOIN EXPOSURE – the paragraph reports that this exposure is related to small head and CNS problems (like hydrocephalus). I'm confused – how can it cause a small head AND hydrocephalus? Only small head? Only hydrocephalus? Please clarify as having both together doesn't make sense since hydrocephalus by default is a BIG head.
- The book is correct, per Medscape.com, Isotretinoin exposure can cause both microcephaly and it can also cause hydrocephalus.
- You are correct in thinking that hydrocephalus can cause a big head in infants as their skull is still growing, however, by definition hydrocephalus is just excess CSF build up in the ventricles deep within the brain and does not always cause macrocephaly. Kids and adults can have hydrocephalus with normal head size.
Page 230 states that Carbamazepine exposure is similar to VALproic acid (Both have spine/facial deformities) and PBR took the time to list both separately. But i don't see a key finding that separates them. Is there one?
- Differentiating between these two is something that you will not likely be tested on. Perhaps they would ask “which birth defect is associated with” X, but given the significant overlap it’s very unlikely that they would ask you to differentiate between these two as answer choices.
==========================================
OPHTHALMOLOGY
p.233 – regarding CORNEAL LIGHT REFLEX TEST – the description under this title is actually referring to the “PUPILLARY light reflex test,” NOT corneal light reflex test. I think the title needs to be changed accordingly to “Pupillary Light Reflex Test.” The Note underneath this section about the Corneal Reflex Test is correct; and there is no “light” used when doing the corneal reflex test. You can probably separate the two tests and have a separate bullet for the Corneal Reflex Test as described by the blink test; without having to explain the name similarities – since the correct descriptions of each test does this already 🙂
- The book is correct, the corneal light reflex uses a light to screen for strabismus vs. pseudostrabismus.
- https://ww2.health.wa.gov.au/~/media/Files/Corporate/general%20documents/CACH/CHM/CACH.CHSH.CornealLightReflexTest.pdf
- https://www.health.state.mn.us/docs/people/childrenyouth/ctc/visionscreen/corneallightreflex.pdf
==========================================
GENETICS
The Translocation Downs section is confusion on page 244: “If you need more information to make it stick in your mind, start by clicking on the link below and just reading the first four paragraphs (then stop!).” is what it says in the book, but the link is broken. Can you go over it please?
- This is confusing and the book will be simplified as seen below:
- * TRANSLOCATION DOWN’S: This is very confusing. Parental karyotyping IS needed. Please start by looking at the shortcut below. So essentially, if the child’s karyotype shows a translocation, get karyotyping of both parents’ chromosomes. The carrier parent will have either the main part of chromosome 21 attached to a different numbered chromosome (usually chromosome 14, in which case this is a partial translocation), or the main part of one chromosome 21 will be attached to the main part of another chromosome 21. The second possibility may be shown as t(21q;21q) and carries a 100% risk of future Translocation Down Syndrome babies because that parent only has that chromosome (21 attached to 21) to donate. The first possibility (in which 21 is attached to 14) carries about a 10-15% chance of future Down’s pregnancies if the MOM is the carrier, and about a 5% if the DAD is the carrier. If you take the time to work out the actual inheritance pattern, it’s theoretically 33%. But nature doesn’t seem to care. In any translocation carrier, that person’s siblings should also be given the opportunity to be screened.
- * SHORTCUT:
Trisomy 21: Age related risk + 1% is the risk of future Down’s pregnancies.
Anything else: < 15% Risk
In reviewing genetics, the information on VACTERL states with hydrocephalus it can be an x-linked disorder. However other sources say it is autosomal dominant with hydrocephalus.
- We have seen mention of a possible autosomal recessive component, but we have NOT seen autosomal dominant. In general, the “When associated with hydrocephalus, this can be an X-linked disorder.” statement in the Core Study Guide is likely a low yield fact because it also seems that there is “no known pathogenetic cause to explain the grouped incidence.” Meaning, we don’t know why it happens. As such, it’s actually called an “association” rather than a syndrome and we might be changing it in the Core Study Guide.
- (DOUBLE TAKE) VACTERL ASSOCIATION (AKA VATER): VACTERL is an acronym. It stands for Vertebral anomalies, Anal atresia/imperforate anus, Cardiac defects (especially VSD), Tracheoesophageal fistula, Radial hypoplasia and Renal anomalies, and Limb abnormalities. These children have a normal IQ.
- PEARL: The patient may present with a single umbilical artery.
- MNEMONIC: Imagine Darth VACTER cutting off his own son’s ARM (radial hypoplasia and limb abnormalities) and then using the ARM as a light saber to create ANAL ATRESIA and a TE Fistula.
IMAGE: pbrlinks.com/VACTERL1
IMAGE: www.pbrlinks.com/VACTERL2
What is the most common cardiac anomaly associated with Turner Syndrome? PBR notes it is Aortic Coarctation. I have run into questions (and further resources) where the answer was Bicuspid Aortic Valve.
- Seems that about 33% – 50% of cases are going to be a bicuspid aortic valve. Coarctation of the aorta is about 20% of the cases. We didn’t state that coarctation is the highest or most common cardiac association, but we don’t mention bicuspid at all. This will be updated as shown below:
- (DOUBLE TAKE) TURNER SYNDROME (AKA TURNERS)
Turner Syndrome (AKA Turners) has a high association with Aortic Coarctation and Bicuspid Aortic Valve. Look for a WEBBED NECK (also called CYSTIC HYGROMA). The patient may have a history of having only breast buds, but they do NOT have breasts. There may be short stature, pedal edema, wide spaced nipples, and short 4th and 5th metacarpals, and may have either scant or no pubic hair. Primary amenorrhea occurs because of streak ovaries and ovarian failure. They DO have a uterus. High FSH always means ovarian failure (top two reasons are Turners and autoimmune ovarian failure) = HYPERGONADOTROPIC HYPOGONADISM. The patient may also have renal anomalies including a possible HORSESHOE kidney. Diagnose by karyotype.
IMAGE: www.pbrlinks.com/TURNER1
IMAGE: www.pbrlinks.com/TURNER2
IMAGE: www.pbrlinks.com/TURNER3
MNEMONIC: Association between XO and coarctation of the Aorta: “XO kind of looks like AO (abbreviation for aorta), doesn’t it?
MNEMONIC: Coarctation of the Aorta and Horseshoe Kidney = In case you didn’t know, Tina TURNER was married to a man who was reportedly abusive. His name was Ike. Now imagine Tina TURNER’S hand thrusting through Ike’s chest and squeezing his AO. He TURNS and hits her in the head with a HORSESHOE!” KEY: Squeezing his AO = Coarctation of the Aorta. Horseshoe trauma = Horseshoe Kidney.
MNEMONIC IMAGE: www.pbrlinks.com/TURNER4
Is fragile X syndrome inherited in X-linked dominant typically? (according to here it is: Fragile X syndrome is inherited in an X-linked dominant pattern.) but in PBR it was under misc so I’m not sure…
- You are correct, it could be in a better location and will be moved to the X-linked dominant section.
==========================================
HEMATOLOGY AND ONCOLOGY
Could you please go over how to differentiate Osteosarcoma vs Growing pains vs Osteoid Osteoma? I tend to confuse these on practice questions. Thank you.
- For growing pains, the nighttime component would likely be mentioned in a vignette.
- For osteosarcoma, it’s often found incidentally on an x-ray after a fall or injury. Once there is pain, NSAIDS don’t improve the pain.
- For osteoid osteomas, the vignette may state that NSAIDS DO improve the pain.
Page 267 (2019). Pearl says alpha thalassemia cannot be definitively diagnosed by hgb electrophoresis (must do genetic testing). Which is it? Hgb electro or genetic testing? Which is the diagnostic test of choice?
- This seems to be a complex topic that you (and we) should probably avoid going too deep into. Here’s a short snippet from the AAFP that confirms what our content says:
- “…a normal concentration of HbA2 does not rule out beta thalassemia trait, especially if there was coexistent iron deficiency, which can lower HbA2 levels into the normal range. In the newborn period, if the electrophoresis shows Hb Bart's or HbH, the infant has alpha thalassemia. The hemoglobin electrophoresis is usually normal in adults with alpha thalassemia trait.”
- Against our better judgment, here’s the link to the “diagnosis” section in case you’d like to investigate further:
- https://www.aafp.org/afp/2009/0815/p339.html#sec-3
Could you please clarify: Is leukocoria in Retinoblastoma usually unilateral vs leukocoria in Cataract bilateral?
- You can have bilateral retinoblastoma OR cataracts, and you’ll have bilateral leukocoria, so you have to look deeper into the history and diagnostics.
Can you please go over anemias, especially quick way to differentiate among the thalassemias, and then among other anemias looking at high vs low retic counts, differences in RDWs? Thank you.
- Alpha vs. Beta Thalassemia is what you’ll see mostly on testing. It’s difficult to know based on counts alone. You’ll need additional information. For Beta, usually you’ll see Indian subcontinent, Asians, middle eastern. For Alpha, you’ll see hydrops with swelling.
- For Beta intermedia or major, look for lots of transfusion to keep themselves alive.
- Iron deficiency, untreated: low hgb, low retic, normal or low RDW.
- Iron deficiency, partially treated: high rdw, retic count a little higher, need iron to develop retics.
- Sickle and thalassemias hemoglobinopathies: Higher reticulocyte count, because has iron around and is trying to compensate by increasing RBCs, hence a higher RDW.
- LAB REVIEWS – FERRITIN, TIBC, RDW, & TRANSFERRIN SATURATION
* FERRITIN:
– Extremely low (< 15) = Iron deficiency anemia.
– HIGH = Anemia of chronic disease or INFLAMMATION
* TIBC:
– High = Iron deficiency anemia
– LOW = Anemia of chronic disease, lead poisoning, and just about anything else.
* RDW:
– Anemia + LOW RDW may mean thaLOWssemia.
– Anemia + HIGH RDW may mean early iron deficiency anemia.
* TRANSFERRIN SATURATION:
– LOW = Low iron
– HIGH = Plenty of iron around to bind the empty sites
For ALL and AML, do we need to know anything about the treatments? Or just tumor lysis syndrome
- Focus more on tumor lysis syndrome on page 260. See PBR for more details.
- TUMOR LYSIS SYNDROME: Tumor lysis syndrome is an ONCOLOGIC EMERGENCY. It occurs due to lysis of large tumors or “blood tumors” (lymphoma). Potassium, phosphorus, and uric acid levels are elevated due to release from lysed cells. Treat with allopurinol or rasburicase, aggressive hydration, and careful monitoring and management of electrolytes. Urine alkalinization by giving sodium bicarbonate is no longer generally recommended.
- Rasburicase should only be used in those without G6PD. If the G6PD status is not known then rasburicase is not used in males. Give allopurinol instead.
- Toxicity of Rasburicase is: Cardiac, liver
How do you treat g6pd deficiency if someone is experiencing hemolysis?
- This is too specific for the boards but depending on the level of hemolysis it is usually self-limited and resolves in 8-14 days. In severe hemolysis, a transfusion may be needed. Always remove the oxidative trigger such as certain medications, foods, and environmental exposures. Look at page 166 in the PBR for all the details that you need to know.
- Glucose-6-Phosphate Dehydrogenase Deficiency (G6PD Deficiency) is an X-linked recessive disorder (so look for a male patient!) resulting in jaundice, dark urine, and anemia due to hemolysis from oxidative injury. In newborns, this will present with jaundice in a MALE baby AFTER 24 HOURS. In other children, it can result in hemolysis after ingestion of fava beans, malaria medications, trimethoprim-sulfamethoxazole, ciprofloxacin, or nitrofurantoin. Look for HEINZ BODIES (purple granules noted in the red cells on microscopy). G6PD Deficiency is associated with patients of African-American and Mediterranean descent.
- PEARL: Do not test for the deficiency during the acute hemolytic phase. Instead, wait a few weeks because a false negative result can occur due to the build-up of G6PD in reticulocytes.
- MNEMONIC: Imagine a bottle of HEINZ BODIES ketchup that has an X located on the exact spot that you have to hit it to make the broken RBCs come out of the bottle. Or, look at this X-shaped HEINZ BODIES bottle of ketchup.
- NAME ALERT: This is not the same as glucose-6-phosphatase deficiency, which can affect glucose metabolism and is associated with glycogen storage disease 1, von Gierke's disease.
ALL = acute lymphocytic leukemia = acute lymphoblastic leukemia, correct?
- Yes, you are correct. We can add a line to the text on page 256 as seen below.
- ACUTE LYMPHOCYTIC LEUKEMIA (ALL) (aka ACUTE LYMPHOBLASTIC LEUKEMIA)
- https://www.cancer.gov/types/leukemia/patient/child-all-treatment-pdq
==========================================
INFECTIOUS DISEASE
For rubella… do you mean: for IMMUNIZED CHILDREN? In PBR it states for rubella that: In unimmunized children who get this infection, it’s generally a benign, self-limited viral illness.
- pg 294 PBR is correct. In immunized or unimmunized children, rubella is a mild illness (fever, sore throat and rash). So a pregnant woman may have a mild illness, but the effect on the fetus could be severe.
I thought for acute sinusitis, we treat with augmentin, can you clarify when we treat with amox vs when we'd treat with augmentin (amox-clav)?
- pg 302, either amoxicillin or amoxicillin-clavulanic acid are fine for first line treatment per the AAP guidelines on acute bacterial sinusitis in children 1-18 years of age.
A needle stick from a HIV patient, is THREE medications, and not two medication like mentioned in the book. PBR states “If you get stuck with a needle from an HIV patient, you get two medications for prophylaxis.”
- pg 293, a 2-drug or 3-drug regimen may be used, though the 3-drug regimen may be preferred. We’ll be doing more research on this for the next edition.
For genital HSV, I thought the treatment is valacyclovir BID x 7-10 days? (not acyclovir)
- Acyclovir, famciclovir and valacyclovir have similar efficacy. Acyclovir is the cheapest and most likely to be tested on the boards. See the update to the book below.
- HERPES SIMPLEXVIRUS (HSV) AS AN STD: The initial flare is often very painful. Pain may precede the presentation of lesions. Look for multiple, painful ulcers or vesicles on the labia or penis. The patient can have lymphadenopathy. The vesicles are CLUSTERED on an ERYTHEMATOUS BASE. Lesions can also be ULCERATIVE. Diagnose by obtaining HSV PCR or a viral culture. The Tzanck smear is not specific for HSV. Treat with ORAL (not topical) Acyclovir x 7 days. Treat babies with IV Acyclovir. Note that valacyclovir and famciclovir are also similarly efficacious, but they tend to be more expensive.
Should we be adding steroids to our treatment of otitis externa? In this chapter, it states “PEARL: You should also GIVE STEROIDS in order to decrease inflammation and edema in order to ALLOW the antibiotic drops to get in and do their job!” However, PREP 2019, NUMBER 148 states that the 2010 Cochrane review found insufficient evidence with the addition of corticosteroid to improve out comes. Mind you, in that question the patient also had perforated TM with otitis externa. The wrong answer was polymyxin B and bacitracin with hydrocortisone (what I picked). The right answer was polymixin B and bacitracin. So my question is, in a patient with otitis externa with intact TM, should we add steroids? I know clinically we do all the time, but what the right board answer? I just memorized that with perf TM and otitis externa we don't add steroids… but the answer didn't go into intact TM and OE.
- It’s not a requirement but giving topical steroids can decrease the time for symptom resolution. On the exam you probably won’t be asked to give antibiotics alone versus antibiotics + topical steroids.
- PEARL: You should also GIVE TOPICAL STEROIDS in order to decrease inflammation and edema in order to ALLOW the antibiotic drops to get in and do their job!
LYMPHOGRANULOMA VENEREUM SEROVAR: Can you treat this with azithromycin? In PBR it says: Treat with DOXYCYCLINE or erythromycin.
- You can, but that’s not first line.
Can a mother of an infant with HSV gingivostomatitis still breastfeed?
- Per the CDC, an HSV+ mom can breastfeed as long as there are no lesions on the breasts and all other lesions are fully covered.
P. 294 under Measles Post-exposure Prophylaxis, the 4th bullet point states: “IVIG is given to any exposed immunocompromised individual regardless of immunization or vaccination status.” –> however on pg. 321 the very top sentence regarding the same subject, it states “Severely immunocompromised patients should be given MIG regardless of their immune status.” **I'm guessing the latter is correct; and the former on p. 294 should say “MIG,” not “IVIG?” Please clarify.
Both are correct and refer to the administration of measles immunoglobulin. Understandably, the confusion came in because we stated “IVIG” rather than IV measles immunoglobulin. For the exam, it’s very unlikely that you’ll be asked to differentiate between IV versus IM immunoglobulin. For the book, we’ve updated the last bullet point to be more clear
- If < 3 days since exposure in an unimmunized child > 6 months old, give the vaccine (MMR). Also give if vaccination status is unknown. If the MMR is given for prophylaxis and the child is 6 to 12 months of age, s/he will need it again at one year of age.
- If > 3 days but < 6 days since exposure in a high-risk, unimmunized child, including those who are immunosuppressed or under 5 years old, give measles immunoglobulin (MIG). Also give this if the patient’s vaccination status is unknown. Anyone given MIG will need a first-time vaccination, or possibly a re-vaccination, 5 months after the MIG dose. No prophylaxis is needed if the child is presenting on, or after, the 7th day after exposure.
- If < 6 days since exposure in a child < 6 months old, give measles immunoglobulin (MIG) only. Anyone given MIG will need a first-time vaccination, or possibly a re-vaccination, 5 months after the MIG dose. No prophylaxis is needed if the child is presenting on, or after, the 7th day after exposure.
- IV measles immunoglobulin is given to any exposed immunocompromised individual (immunodeficiency, on chemo, low CD4, etc.), regardless of immunization or vaccination status.
Just did a Board Vital question regarding treatment of C. difficile infection with a first recurrence and in the answer stem it stated: “For a first recurrence, vancomycin or fidaxomicin should be used if metronidazole was used initially.” According to PBR a first recurrence should be treated with the same medication initially used. So in this case Metronidazole should have been repeated. These two statements are in conflict with each other, which is correct?
- We’ve reviewed the latest recommendations and are happy with what we have. Please use the Core Study Guide to guide your decisions on the exam for this topic.
==========================================
VACCINES, IMMUNIZATIONS, AND CONTRAINDICATIONS
This topic is approached in both the Vaccination Chapter and ID chapter and the two sections have differences. Page 294 and Page 320.Pg. 294 – Vaccinate for > 6 month old and between 1-3 days of exposure; Pg 320 – vaccine or MIG. I am assuming page 320 is correct with either MIG or Vaccination within 78 hours.
- The content is correct on page 320. For complicated sections such as this create summary notes like mine below to study over and over again or come up with a mnemonic to help you remember the details. Look for patterns and use highlighters and notes in the margins. I find that by creating my own notes off PBR that I learn the material better. Try to teach it to someone. Find a study group or use the PBR Facebook page to connect with other members and set up WhatsApp conference calls to quiz each other.
- Measles exposure < 6 months old -> MIG
- >/= 6 months and Measles exposure < 72 hours prior -> MMR (only if unvaccinated) or MIG
- >/= 6 months and Measles exposure 72 hours to 6 days -> MIG
- >/= 6 months and Measles exposure > 6 days -> No prophylaxis is indicated
Notes:
- DO NOT GIVE MMR for at least 5 months after giving MIG
- DO NOT GIVEN MMR and MIG at the same time
- If the child is < 1 year and receives the MMR, then they will need another MMR according to the routine vaccine schedule
For an unimmunized child , 7yo or older , do they need both Tdap and Td ?
- Just Tdap starting at age 7 years, second dose is 4 weeks later, followed by 3rd and final dose 6 months later. https://www.cdc.gov/vaccines/schedules/hcp/imz/catchup.html
==========================================
INBORN ERRORS OF METABOLISM
Can you go over why calcium channel blockers do not work in children with hypoglycemia due to hyperinsulinism?
- It’s not clear in the literature. We’d suggest simply taking these kinds of tid bits of information at face value unless you think that the PBR content is incorrect. However, I’ll take a stab at it. Calcium channel blockade inhibits insulin release, which seems like it would help in a hyperinsulinism state, however, given that glucose is already depleted from the cells due to the hyperinsulinism state, this just makes hypoglycemia worse.
- https://www.medscape.com/answers/2184611-167346/what-is-the-role-of-insulin-therapy-in-the-treatment-of-calcium-channel-blocker-ccb-toxicity
In the past I have noted geneticists or neurologists ordering organic acids and amino acids. Is this something that should be done by the general pediatrician also?
- For the purposes of the exam, the amino acids and organic acids mentioned in our content would be fair game. Anything beyond that would not.
p.330 – under FATTY ACID OXIDATION DISORDERS – the PEARL states: “If given an answer choice with a disease that has “CARNITINE” in the name of it, that IS a fatty acid oxidation disorder.” I think the word you were looking for was not “Carnitine,” but “Acyl-Co-A,” or “Acyl-coA dehydrogenase,” correct? Because all of these disorders (medium chain/long chain/very long chain acyl-coA dehydrogenase), have this word in it.” Please correct.
- Both CARNITINE and Ac-Co-A dehydrogenase are correct. There are several disorders of FAO, including defects in the carnitine shuttle, which is how fatty acids are transported across the mitochondrial membrane. Examples include defects in: Carnitine palmitoyltransferase I (CPT I), carnitine-acylcarnitine translocase (CACT) and carnitine palmitoyltransferase II (CPT II. Other disorders are in the “acyl-CoA dehydrogenase” family.
- From a test-taking strategy point of view, Acyl-CoA dehydrogenase would be too obvious, so I think the pearl of looking for the word “carnitine” is helpful, but perhaps not the only possibility.
Page 328/329 – In re: Urea Cycle defects/deficiency, there are 4 disorders listed on 328: OTC deficiency, Citrillinemia, Arginosuccinic aciduria and Carbomyl Phosphatase Synthetase deficiency BUT the table summary does not include Carbomyl synthetase deficiency. I am correct to assume that it would look just like OTC deficiency (since part of same reaction) and only difference would be inheritance i.e. if xlink OTC?
- Yes, carbamyl phosphate synthetase is a part of the same reaction as OTC so would have the same findings as OTC deficiency. ORNITHINE TRANSCARBAMYLASE works with CARBAMOYL PHOSPHATE SYNTHETASE to catalyze the reaction between AMMONIA and ORNITHINE to create CITRULLINE!
| OTC DEFICIENCY | |
| CITRULLINE LEVEL | LOW |
| ARGININOSUCCINIC ACID LEVEL | LOW |
| ARGININE LEVEL | LOW |
| URINE OROTIC ACID LEVEL | HIGH |
==========================================
ACID-BASE DISORDERS
p.345 – under CHLORIDE RESPONSIVE – you describe vomiting, dehydration and diuretics as Chloride-responsive metabolic alkalosis. However, in the 2nd PEARL – you mention “LAXATIVES, diuretics and excessive vomiting all cause hypokalemic, hypochloremic metabolic alkalosis.” I think you meant to say “DEHYDRATION, diuretics and excessive vomiting…” correct? Since those are the main 3 that cause CL-responsive metabolic alkalosis. Because we all know Laxatives cause us to lose bicarb – loss of bicarb leads to metabolic ACIDOSIS, not alkalosis. Please correct.
- Laxatives cause alkalosis not acidosis, which is already in the PBR text, so no correction needed.
- https://www.mdedge.com/ccjm/article/96062/adolescent-medicine/recognizing-managing-medical-consequences-eating-disorders/page/0/2 (reference 48 of this article explains the question pretty well)
On page 345 of the study guide- it first says urine chloride is high in diarrhea (>15) (under the last part of the RTA section) but then under the chloride-responsive metabolic alkalosis section, it states laxatives and dehydration can cause urine chloride <15. The latter is consistent with what I google too. is the part about urine chloride being high in diarrhea a typo?
- The book is correct. In diarrhea, there is a non-gap metabolic acidosis and the kidneys are just fine, so think of them getting rid of HCl (mnemonic). So urine Cl is HIGH. The key for chloride responsive metabolic alkalosis is that the body is STARVING for chloride and holding onto as much as possible, thus the urine Cl is LOW. Dehydration causes a contraction alkalosis through multiple mechanisms in the kidney in an effort to compensate. It’s especially bad when you are already vomiting out HCl! With loop diuretics and thiazides, but only if there is insufficient dietary chloride (like in a patient on NaCl/salt restriction). If a metabolic alkalosis is given in a patient on a diuretic, the patient will also likely have a concurrent hypokalemia.
Can you provide an example using winter's formula?
- Winter’s formula is used to predict the PCO2 in a patient with a primary, overarching metabolic acidosis.
- Predicted PCO2 = (1.5 x BICARB) + 8 +/- 2So if the bicarbonate level is 20, then 1.5 x 20 is 30.30 + 8 = 38
- The range of a compensated PCO2 would be +/- 2, so 36-40. A HIGHER PCO2 would represent a concurrent, primary respiratory acidosis.
- A LOWER PCO2 would represent a concurrent, primary respiratory alkalosis.
- If you’re an Online Video Course member, click here and watch a 26-minute video on acid-bases, which includes the practice of 6 acid-base questions.
==========================================
FLUIDS AND ELECTROLYTES
Under DAILY FLUID REQUIREMENT – the units for fluid are written wrongly as ml per day – should be ml/kg/day. For example, it should say: “100 ml per kg per day for each of the first 10 kg…or more easier; as 100 ml/kg/day.” In these number-based or math-based questions, it's MUCH easier to understand and memorize when concepts are written in shorthand; (ml/kg/day) rather than in paragraph (ml per kg per day) – just an FYI.
- Good catch, we will change to 100 ml/kg/day for the first 10 kg + 50 ml/day for each of the….
[IMAGENEEDED] – 59
Can you please go over SIADH and CSW (cerebral salt wasting)? I get confused. My understanding is SIADH = low urine output and hypervolemia, vs. CSW = hypovolemia…. how would I be expected to apply that concept to a question/clinical scenario? Thank you.
- Longer discussion than a quick response would justify. For bigger picture, refer initially to PBR. Briefly, SIADH is a disorder of water retention, while CSW is a disorder of uncontrolled excretion of sodium due to brain disease. SIADH by definition is low urine output (or low-normal), low serum sodium, normal-high urine sodium (i.e. inconsistent with serum sodium), low serum osmolarity, high urine osmolarity. I wouldn't use “hypervolemia” as a buzzword. Salt-wasting is exactly what it sounds like – sodium is lost uncontrolled, and water follows, leading to high urine output, with low serum sodium, very high urine sodium, and significant fluid losses leading to hypovolemia. SIADH has multiple causes, including surgery, critical illness, spinal injury, cancer. CSW is usually a consequence of severe brain injury but can happen after brain surgery as well. Board questions should include a possible etiology, with a pattern of urine and serum labs that include volume of urine output.
I am having difficulties with calculating the amount of IVF mL/hr of ____ fluid (I am assuming a hypertonic fluid likely 3% NaCl IVF) when correcting for hyponatremia. I think where I get confused is how you go from using the formula where you calculate how many meq of sodium is needed per kg of weight to the mL/hr for the particular IVF. Would it be possible to have a break down of the math and how the meq sodium gets converted into mL/hr of 3% NaCl IVF over how many hours?
For example – if you need 10mEq of sodium per kg of weight to raise the sodium by 12 meq/L over the next 24 hours –> what would that be in mL/hr of 3% NaCl IVF? I feel like this is good to know for the test (I had one question like this in one of my question banks, but I unfortunately cannot find it, but I remember that it did not break down the answer very well), as well as for real life if a patient comes in hyponatremic.
Thank you so much for your time and assistance!
The formula I am referring to is found on p.351 of PBR 9th edition.
- Very good question, but this is beyond the scope of the pediatric boards. Please know the pearls below and that should be sufficient.
- PEARL: Formula to correct = (desired Na – measured Na) x Weight in kg x 0.6. Then ADD 3 mEq/kg as the daily maintenance amount of sodium needed. This will give you the total amount of sodium needed for the next 24 hours to reach the desired sodium level you input into the equation, which should never be greater than 12 above the measured sodium. So, if measured is 115, desired should be no more than 127.
- SHORTCUT: If the desired change in sodium is 12 mEq over 24 hours, then 12 x 0.6 = 7.2, and a simpler formula for the correction of sodium = (7 x Weight in kg) + (3 mEq x Weight in kg). Using basic algebra, this comes out to 10 x Weight in kg. So, 10 mEq of sodium is needed per kg of weight to raise the sodium by 12 mEq/l over the next 24 hours. This formula includes the sodium needed for maintenance. It does NOT calculate what kind of sodium-containing solution is needed, or how much water should be given. Those can vary depending on the clinical scenario, for example, the degree of estimated dehydration.
Can you explain the mechanism as to why hydrochlorothiazide, a diuretic, is used for treatment of this condition when there is already massive urine output. I understand that DDAVP/ADH won't work given that the receptors are either partially or completely non-functional, and I understand that salt/protein restriction will be required, but the diuretic seems counterintuitive. Thanks in advanced for the help.
- I assume that you are asking about nephrogenic DI. Treatment is aimed at minimizing the polyuria and avoiding hypernatremia and volume depletion. The mechanism by which hydrochlorothiazide helps to decrease urine output is actually unclear, though there are several theories. In medical school, I was taught that it has to do with the changes created towards the end of the loop of Henle which then paradoxically increase water retention in this particular situation.
- NEPHROGENIC DIABETES INSIPIDUS: Usually X-linked recessive, so look for a male patient. He will have evidence of DI (massive urine output) but will have NO response to DDAVP/ADH supplementation. Water is lost, and the labs will show hypernatremia. Treat with hydrochlorothiazide and salt restriction.
- https://www.uptodate.com/contents/treatment-of-nephrogenic-diabetes-insipidus
Can you go over the difference between hypocapnea and tachypnea?
I understand hypocapnea = low pCO2 = hyperventilation; likewise, hypercapnea = high pCO2 = hypo ventilation; and tachypnea, I should think metabolic acidosis.
The part that confuses me is, increase RR = tachypnea = metabolic acidosis, which has low bicarb – but their pCO2 can be normal (is my understanding).
So with with hypocapnea = low pCO2 = resp alkalosis.
So to be clear, hypocapnea =hyperventilation = resp alkalosis
Whereas, tachypnea = increase RR = metabolic acidosis
If a patient is breathing fast, with increase RR and having metabolic acidosis… so pH is low (the reason they're breathing fast is to blow off the pCO2 in order lower their pCO2 and thereby increasing their pH… So would it be correct to say, someone who's tachypneic – the teaching is think about someone with metabolic acidosis, who is now having compensatory resp alkalosis, and that's why they're breathing fast?
Sorry for long question… I feel as if I'm missing something fundamental in understanding this.
- A respiratory alkalosis can be caused by basically anything that causes tachypnea. Sometimes this is due to hypoxia. The list includes, but is not limited to, early asthma, pneumonia, one of the aspirin phases, high altitude, fever, and anxiety/hyperventilation.
- PEARL: –CAPNEA refers to how much CO2 is in the blood and is NOT referring to how fast someone is breathing. So, hypOcapnea means there is low CO2 in the blood, and this occurs due to HypERventilation. Therefore, you get a RESPIRATORY ALKALOSIS and a compensatory non-gap metabolic ACIDOSIS. HypERcapnea means there is high CO2 in the blood, and this occurs due to hypOventilation. Therefore, you get a RESPIRATORY ACIDOSIS and a compensatory metabolic ALKALOSIS. Make sure you look carefully at the terminology in the question stem or vignette.
==========================================
NEPHROLOGY
UTIs – is cefotaxime IV still considered a good choice given shortage x 2 years? what is the likely treatment for inpatient therapy for UTI prior to sensitivities returning?
- For the inpatient side, we’d recommend IV ceftriaxone as mentioned in the PBR Core Study Guide.
What kind of crystals do you get with ethylene glycol poisoning? rod shaped crystals or maltese cross shaped crystals?
- Calcium oxylate crystals. The ones that are rod shaped. See PBR.
Why is it that in nephrotic syndrome i.e. MCD we use ACEI for HTN, whereas in acute GN we use Loop Diuretics? I'm afraid of getting a question wrong in this regard because I don't understand why we choose one over the other.
- This is beyond the scope of the pediatric boards; the book is correct and please use it as your primary resource. With that said ACEI’s reduce proteinuria in nephrotic syndrome and are the medication of choice for HTN and for acute glomerulonephritis a loop diuretic is preferred as salt and water needs to be restricted and loop diuretics increase urinary output and improve HTN and cardiovascular congestion. ACEI’s and calcium channel blockers are also acceptable in acute GN.
- https://emedicine.medscape.com/article/244631-medication
- https://emedicine.medscape.com/article/240337-medication
==========================================
STATISTICS
Book: Q&A #31-33
Question: The numbers for the calculations are even in the table provided in the answer which led me to get the wrong totals for the answer
Correct values for the table should be:
Total tested = 120
TP = 80
FP = 10
Total positive = 90
TN = 25
FN = 5
Total Negative = 30
Sensitivity = TP/(TP+FN) = 80/(80+5)= 94%
Specificity = TN/(TN+FP) = 25/(25+10)= 71%
PPV = TP/(TP+FP) = 80/(80+10)= 89%
PPV = TN/(TN+FN) = 25/(25+5)= 83%
Unless I'm not reading the question correctly, which if that's the case please help me get it right. I'm bad at statistics
- Thank you so much for submitting this question. The book is correct, and we took the time to go through all 3 of the questions in a live format during our Online Video Course webinar. It was a great discussion about the 2×2 table and how to use it. The replay is currently available at https://members.pediatricsboardreview.com/ovc-schedule (just click STATISTICS).
p.366 – under the Validity Hierarchy title, the order of validity listed is missing ‘Cross-Sectional Studies.” The hierarchy should instead read: Systematic Review and Meta-Analysis >> Randomized Controlled Trials >> Cohort Studies >> Case-Control Studies >>Cross-Sectional Studies >> Case Studies. Please clarify.
- Sure, we can update this list to include Cross-sectional studies. See update below.
- Systematic Review and Meta-Analysis >> Randomized Controlled Trials >> Cohort Studies >> Case-Control Studies >>Cross-Sectional Studies >> Case Studies.
- https://libguides.winona.edu/c.php?g=11614&p=61584
==========================================
NEUROLOGY
No Clarifications! But the 2020 Pediatrics Board Review Study Guides May Have New Content (Or Corrections).
==========================================
ORTHOPEDICS AND SPORTS MEDICINE
If SCFE is a Salter Harris I fracture, then could I assume that if I see a supracondylar fx that it’s a Salter V?
- The Salter Harris classifications specifically refer to fractures that involve a growth plate. In a Salter Harris V fracture, the growth plate is crushed. If the patient no longer has a growth plate, or if the fracture does not include the growth plate, then this classification system is not relevant.
==========================================
RHEUMATOLOGY
Is anti-Smith the same thing as anti-Ro, or anti-La?
- No, they are not the same thing. Anti-Smith is the most specific antibody for lupus and anti-Ro/La Abs are found in people with systemic lupus and Sjogren’s Syndrome.
- https://www.hopkinslupus.org/lupus-tests/lupus-blood-tests/
==========================================
PULMONOLOGY
Is there any one place in PBR materials — core study guide, atlas, elsewhere? — where the high yield CXRs for Pulmonology Chapter are lined up side-by-side, easy to look at to see quickly the differences among pathologies? Or another easy to use resource? PNA, Viral v Consolidation, Mass, Asthma, TB, Atelectasis, Meconium, TTP, RDS, BPD, Pneumothorax, Alpha 1, FBO, etc. I sometimes am confused sorting through nuances of the various CXRs. I understand it is “data block” but quick view of picture can tell the story. Thank you.
- Great chest x-ray atlas resources below
- https://www.radiologyeducation.com
- https://www.seattlechildrens.org/healthcare-professionals/education/radiology/pediatric-chest/
- https://accessemergencymedicine.mhmedical.com/content.aspx?bookid=573§ionid=42496374
==========================================
PSYCHIATRY AND SOCIAL ISSUES
No Clarifications! But the 2020 Pediatrics Board Review Study Guides May Have New Content (Or Corrections).
==========================================
ETHICS
“Mature minors can self-consent.” We describe minors as not having “complete competency” and we described in the ethics section that only those that are competent can give consent. I know we talked about 16yo as a cut off for age of consent, but I feel as if I'm missing something here…. I'm having trouble with the exam definition of consent as it pertains to competency.
- The PBR Core Study Guide doesn’t give 16 years of age as a definitive cut off. Also, the phrase “complete competency” is not mentioned in the Core Study Guide, so perhaps there are mixed resources being studied? Regardless, let’s try to help!
- There are 2 board concepts here to discuss around the idea of the “emancipated minor” and that of a “mature minor.” Additionally, we’ll briefly discuss the idea of competency.
- An emancipated minor can LEGALLY function as an adult (is married, is in the military, has a child, or is living independently).
- A mature adolescent under the age of 18 who does not fit the definition of an emancipated minor may still make certain decisions without parental consent as long they are competent.
- Those certain decisions tend to fall under the areas of STD diagnosis, obtaining contraception, obtaining prenatal care, and obtaining treatment for substance abuse. Also, it is reasonable to allow minors to make other adult-like decisions if they seem mature, competent and if the treatment involves a small degree of risk.
- Other areas (abortion, mental health services, sterilization, etc.) are gray or variable by state and should not be tested by the ABP.
- Regarding competency, the easiest way to understand this concept is to think in terms of medical CAPACITY versus legal “Capacity” has to do with your ability to process the information and make decisions accordingly (this is a medical determination), while “competency” is a legal determination around whether or not a person has the right to make their own decisions, and it is often guided by a clinician’s CAPACITY assessment.
==========================================
PATIENT SAFETY AND QUALITY IMPROVEMENT
No Clarifications! But the 2020 Pediatrics Board Review Study Guides May Have New Content (Or Corrections).
==========================================
PEDIATRIC LAB VALUES
No Clarifications! But the 2020 Pediatrics Board Review Study Guides May Have New Content (Or Corrections).
==========================================
PEDIATRIC VITAL SIGNS
No Clarifications! But the 2020 Pediatrics Board Review Study Guides May Have New Content (Or Corrections).
========================================================================
AWESOME! YOU’RE DONE! – WHAT NOW?
- Read the PBR “Exam Day” article. It’s a MUST read. It will give you a great deal of insight into your exam day. I’ll list the link at the end of the document.
- Go back to your core PBR study material! At the end of the day, THAT is what will help you pass the boards.
- If you’re not a PBR member yet, this is a GREAT time to join!
- If you’re feeling pretty good about your pediatric KNOWLEDGE/CONTENT, then work on your TEST-TAKING STRATEGY by going through the CRASH COURSE on Test-Taking Strategies (it has been a HUGE HIT)!
Pediatrics Board Review…
YOUR RESOURCE FOR EFFICIENCY IN STUDYING…ESPECIALLY DURING CRUNCH TIME!
As the final days of preparing for the initial certification exam come up, there’s often a sense of PANIC. Please BREATHE! If you’ve been studying the PBR thoroughly and you have a fair handle on your test-taking skills, you should be in GREAT shape!
What can you do to MAXIMIZE your remaining study time? Go over your PBR over and over again. Focus on the areas that you still need to master and SKIP the areas that you know well.
Get the DOWNLOADABLE MP3 audio course from PBR so that you can eat, sleep and breathe PBR no matter where you are. Yes… even between seeing patients!
www.PediatricsBoardReview.com/MP3
You can also WATCH 31 videos that cover ALL of the PBR through PBR’s Online Video Course, Conference & Live Webinars in a single day!
www.PediatricsBoardReview.com/VIDEOS
You’ll get chapter videos PLUS our webinar replays for the 2017 Summertime Q&A Webinars.
For the Acid Base chapter, I’ve even included a short impromptu practice question session as well as additional practice questions for our Online Video Course and All Access Pass members to enjoy.
The Acid Base discussions and resources show how confused pediatricians are about the delta delta, when to check for compensation, Winter’s formula, etc… but by these talks and practice sessions, we get comments like, “This is so much easier!… The light bulb just went off!”
www.PediatricsBoardReview.com/VIDEOS
And if you want to CRANK THROUGH the videos and webinars in just 12-14 hours, you can do so at double speeds using our SPEED CONTROL function.
Okay! That’s it!! Now go study in whatever way is going to give you the MOST REPETITION AND LEARNING.
Now go study in whatever way is going to give you the MOST REPETITION AND LEARNING. If that’s simply reading over and over again, GREAT!
PBR 12-MONTH ALL ACCESS PASS + BONUSES(PROMO CODE: PREORDER)
During our 2019 PREORDER Window, PBR is Offering theFollowing VIP Resources with the PBR All Access Pass
**90-Day Personalized Study Schedule Created by Team PBR****CORE CONCEPTS in Test-Taking Strategies Webinar**
HERE'S EVERYTHING YOU GET IN A PBR 12-MONTH ALL ACCESS PASS PREORDER
- Hardcopy Core Study Guide
- Hardcopy Q&A Book
- Online Core Study Guide
- Desktop-Compatible, Mobile-Compatible, Searchable!
- Online Q&A Book
- MP3 Streaming Course
- MP3 DOWNLOADABLE Course
- ONLINE VIDEO COURSE
- Private Facebook CREW Access
- (BONUS) CORE CONCEPTS in Test-Taking Strategies Webinar
- Free Expedited Shipping
- 7-Day Access to the Core Concepts inn Test-Taking Strategies Webinar
- Online Picture Atlas Not Available in Our Catalog Area
- Downloadable PDF Picture Atlas
- Not Available in Our Catalog Area
- Live Summertime Q&A Webinars with Content Experts
- Not Available in Our Catalog Area
- 16+ HOURS of Pre-Recorded Coaching Webinars
- Not Available in Our Catalog Area
- (VIP BONUS) 90-Day Personalized Study Schedule Created by Team PBR
- Not available in our Catalog Area
First-Time Money Back PASS Guarantee
Click Here Now & Signup Before the Offer Ends!
INCLUDES FREE Shipping
http://pbrlinks.com/preorder-aap
Promo Code: PREORDER(Limited-Time Offer)(New Orders Only)
PBR FOR LIFE!
During Our 2020 Edition PREORDER Window, PBR is Offering
- Hardcopy Core Study Guide
- Hardcopy Q&A Book
- Online Core Study Guide with LIFETIME Access
- Online Q&A Book with LIFETIME Access
- 50% Off of All Future Hardcopy Editions of the PBR
- FREE EXPEDITED SHIPPING
First-Time Money Back PASS Guarantee
Click Here Now & Signup Before the Offer Ends!
WITH FREE Shipping
Promo Code: PREORDER(Limited-Time Offer)(New Orders Only)
Ultimate Bundle Pack
During Our 2020 Edition PREORDER Window, PBR is Offering FREE SHIPPING & AN ADDITIONAL DISCOUNT!
- Hardcopy Core Study Guide
- Hardcopy Q&A Book
- Online Sore Study Guide
- Desktop-Compatible, Mobile-Compatible & Searchable!
- Online Q&A Book
- Online Access for 1 Full Year
- GET FREE SHIPPING
- LIFETIME Online Access
- 50% Off of All Future Hardcopy Editions of the PBR
LOCK IN 2019 PRICING & GET IMMEDIATE ONLINE ACCESS
First-Time Money Back PASS Guarantee
Click Here Now & Signup Before the Offer Ends!
Promo Code: PREORDER(Limited-Time Offer)
(New Orders Only)
===
HAVE YOU FAILED?
If you have failed while feeling as though you had a strong handle on the content, it’s likely that you have a test-taking technique issue. Reach out to us and ask about our Test-Taking Strategies course which covers test-taking skills, test-day planning, anxiety management, diet and much more. We also offer LIVE coaching courses
www.PediatricsBoardReview.com/STRATEGIES
Lastly, don’t forget to read some excellent information about your exam and how you should structure your big day. The article below is a MUST read, so please click the link below and take 5 minutes to read it:
www.PediatricsBoardReview.com/EXAMDAY
GOOD LUCK!
From everyone here at Team PBR, we hope that our efforts have been well-received. Your success is truly our primary focus, and we hope that we’ve supported you successfully throughout this journey.
Please finish off with a ton of energy as you go through another round of content review and several strong test-taking strategy sessions.
You’re going to do great!
Trust me, if I can do it… so can you!
Best of luck on your board exam!
Sincerely,
Ashish & Team PBR